Resorption is a condition associated with either physiologic or a pathologic process resulting in a loss of dentin, cementum, and/or bone. (1) The etiology for resorption initiates from various injuries to the tooth, including thermal, mechanical, and chemical. (2) There are two different kinds of resorption — external and internal. External resorption is resorption initiated in the periodontium and initially affecting the external surfaces of a tooth — may be further classified as surface, inflammatory, or replacement, or by location as cervical, lateral, or apical; may or may not invade the dental pulp space. (1) Internal resorption is an inflammation process initiated within the pulp space with loss of dentin and possible invasion of cementum. (1) This review will focus on internal resorption.
ALSO BY DR. STACEY SIMMONS |How I learned to enjoy endodontics
The pathology of internal root resorption (IRR) is caused by transformation of normal pulp tissue into granulomatous tissues with giant cells, which resorb dentin. (3) This, in turn, resorbs the dentinal walls, advancing from the center to the periphery. There are two classifications of internal resorption: internal root canal inflammatory resorption and internal root canal replacement resorption. (2)
- In the inflammatory resorption, the resorptive process if the intraradicular dentin progresses without adjunctive deposition of hard tissues adjacent to the resorptive sites. The phenomenon is associated with the presence of granulation tissues in the resorbed area and identifiable with routine radiographs as a radio clear zone centered on the root canal.
- In the replacement resorption, the resorptive activity causes defects in the dentin adjacent to the root canal, with concomitant deposition of bone-like tissue in some regions of the defect. It results in an irregular enlargement of the pulp space with partially or fully obliterated area of the pulp chamber.
Trauma and pulpal inflammation/infection are two of the major contributory factors in the initiation of internal resorption. (2) Caliskan et al. reported that in a study done on patients diagnosed with IRR, 43% of the patients had trauma as a common etiological factor, followed by carious lesions at 25%. (2,4)
ALSO BY DR. STACEY SIMMONS |We can't save them all: the missing endodontic diagnosis
Internal root resorption is typically detected clinically via routine radiographs. It is observed in all areas of the root canal, but it is most commonly discovered in the cervical region of the tooth. (3) One of the key ways to diagnose internal resorption (vs. external resorption) is to observe whether or not there is a defined outline of the pulp chamber. If the pulp chamber outline is within the lesion itself, it is likely internal resorption. If the pulp chamber outline is recognizable within a radiolucent halo, then it is likely external resorption. The use of CBCT has allowed for more accurate and complete diagnosis of IRR (and external root resorption) and is highly recommended in early presentations of potential resorption. (2,3)
IRR is usually asymptomatic, but pain or discomfort may be the chief complaint if the granulation tissue has been exposed to oral fluids. (3) The granulation tissue can clinically manifest itself as a “pink spot” where the crown dentin destruction is severe. (3) The pink shade is related to the highly vascularized connective tissue adjacent to the resorbing cells and when the pulp becomes necrotic, it turns grey/dark grey. (2)
Teeth with IRR typically respond normally to pulpal and periapical tests until the lesion grows significantly in size, which then results in perforation. (2,5) Once necrosis of the pulpal tissue takes place, then the typical signs/symptoms of an abscessing tooth occur. Vital pulp tissue is required for IRR to take place; therefore, when there is complete pulpal necrosis, the growth of the resorption ceases because the resorbing cells are cut off from the blood supply and nutriments. (2,3)
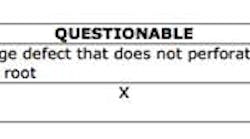
Once diagnosed, treatment considerations and prognosis must be rendered. Since removal of vital tissue ceases progression of the lesion, then initiation of root canal therapy is recommended. However, the prognosis for the long-term form and function of the tooth is dependent on the size of the lesion. The American Association of Endodontics (AEE) offers this as a general guide: (6)
Case report
A healthy 36-year-old male presents to the office with a chief complaint of a loose front tooth. A radiograph revealed significant bone loss around tooth No. 10 in addition to the focalized loss of internal tooth structure in the apical one-third of the root. Obvious perforation of the root was observed. Clinical exam revealed a lack of recession, probing depths of 8+ mm with a Class III mobility. No drainage point or fistula were noted. The patient indicated that he had the crowns placed in the anterior area eight years ago and has not had any complications since then. He furthermore admits to lack frequent dental visits during this time.
Differential diagnoses of internal and external resorption were given. Earlier radiographs would definitely aid in a more accurate and definitive diagnosis, but ultimately, internal resorption was given due to the focal point of radiolucency within the pulp chamber area. While there could be debate on this, the ultimate fate of the tooth did not change. Due to the extent of the defect (perforation through external root surface) and the advanced bone loss and periodontal disease, it was recommended that that tooth be removed and other restorative options be assessed. Upon removal of the tooth, there was very little root structure left as it came out in a multitude of pieces.
Internal root resorption is observed daily in practice (although more rare than external resorption) and with early detection (especially with the use of technology and CBCT scans), diagnosis, and management, the prognosis for rendered treatment can be favorable. The numerous resources available offer significant aid in the diagnosis and treatment of such lesions.
References
1. American Association of Endodontics, “Glossary of endodontic terms,” 2014. www.aae.org/glossary
2. Nilsson E, Bonte E, Bayet F, Lasfargues J. Management of internal root resorption on permanent teeth. International Journal of Dentistry. Volume 2013. Article ID 929486, 7 pages.
3. Maria R, Mantri V, Koolwal S. Internal resorption: A review and case report. medind.nic.in/eaa/t10/i1/eaat10i1p98.pdf
4. Caliskan MK, Turkun M. Prognosis of permanent teeth with internal resorption: A clinial review. Dental Traumatology. 1997;13(2):75-81.
5. Principals and Practice of Endodontics. 2nd Edition. Walton & Torabinejad. WB Saunders Company. 1996. 36.
6. American Association of Endodontics website. www.aae.org/treatmentoptions. Internal Resorption.