An endodontist answers 8 questions GPs ask about root canal treatment
Due to the time constraints and complexities of root canals, many dentists refer patients to colleagues or bring in an in-house endodontist. Iman Sadri, DDS, spoke with Moji Bagheri, DMD, an endodontist who practices in Southern California, to gain further insight into the dynamic world of endodonics and seek his answers to questions GPs ask about root canal treatment.
I believe root canals will remain a viable option for restoring the dentition that have sound tooth structure, despite the changing landscape of clinical dental care as it seeks to focus on implant dentistry. As long as there is dental care, there will be a need for root canal treatment. Due to the time constraints and complexities of these procedures, many general practitioners refer their treatment-planned root canals to their specialist colleagues or bring an in-house endodontist to their office. As dentistry continues to evolve with advanced optics and materials, so does the field of endodontics.
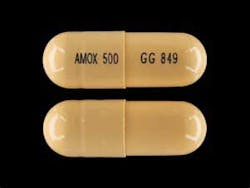
1. What is the most common antibiotic you prescribe and why?
My first choice of antibiotics is amoxicillin—that is, if there are no contraindications, such as allergies (figure 1). Because of its broad spectrum, it is effective against root canal-invading bacteria and polymicrobial infections. Metronidazole is added to the regimen if amoxicillin is ineffective after 48–72 hours. This combination, based on studies that have been done, (1) has an efficacy of 99%. In case of a penicillin allergy, I prescribe clindamycin.
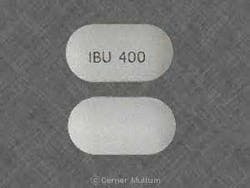
2. What are the common analgesics you prescribe after endodontics and why?
I prescribe NSAIDs, such as high-dose ibuprofen, after all root canal treatments and have patients take the first dose usually prior to anesthesia wearing off (figure 2). The rationale is such that after most root canal treatment there is a moderate amount of inflammation present around the tooth and in the supporting bone and periodontal tissues. This inflammation can be alleviated by blocking the production of inflammatory mediators responsible for pain and inflammation in the blood, such as prostaglandin and thromboxane A2, thus reducing inflammation and pain at the local site. Another very important and often-overlooked factor—and, in my opinion, goes hand in hand with the analgesic effect—is the occlusal force that is applied to the treated tooth post-op. By eliminating such occlusal pressure, the already-inflamed supporting structures of the tooth have a chance to heal without interruption from occlusion and, therefore, potentially heal faster.
3. Which teeth do you do the most root canals on, and why do you think these are the most common?
In the past couple of years, the most common root canals I do have been the upper and lower molars, especially second molars. I think there are several reasons for that. The location of the teeth, being far back in the upper and lower arches, make access to them difficult, especially the upper seconds. This difficult access leads to difficulty in negotiating the canals and performing the root canal treatment. There are situations when the patient has an existing full-coverage restoration that makes it especially challenging, because the original landmarks of the tooth are gone, and access and locating the canals rests solely on pulp chamber anatomy and operator experience. The lower molar could potentially be less difficult, because you have the advantage of direct vision and less anatomical limitation for a proper isolation. Another reason that the second molar is more commonly treated is that throughout the life of the tooth, there is more of a chance of damage to it from decay and plaque buildup. Maintaining hygiene in this area is more difficult and needs more attention; therefore, there is a greater chance of having a root canal done during the life of this tooth. And let’s not forget—second molars are referred to me the most!
Tooth pain after root canal therapy: The 5 common causes
4. You have stated before that retreatment of failed root canals is the most common treatment you do. Why do you see failed endodontics from GPs, especially on root canals that appear to look good radiographically?
As I mentioned before, I think the most important aspect of root canal treatment is the criteria for case selection by the practitioner. I think the GP who chooses to perform a procedure should be well aware of his or her limitations and skills, as well as what is best for the patient. Several of the reasons that we see failures in root canals done by GPs include:
- Improper amount and type of irrigation.
- Improper use of the rubber dam and/or poor isolation. It is essential to keep the area as sterile as possible.
- Improper selection and use of obturation material and techniques. A material such as Thermafil is very technique sensitive and if not used properly would certainly lead to root canal failure. Once obturated, it may appear excellent on the radiograph with the material seemingly filled to the apex, but you could see the presence of a large periapical radiolucency on the radiograph in a failed case, which could indicate potential loss or no seal at the apex.
The myth of "easy" root canals
5. What is the average time that you spend irrigating on molars? Is it the same for maxillary and mandibular?
The irrigation is usually performed throughout treatment from the time it is accessed and right up to the point where obturation is to occur. A final irrigation is done anywhere from one-to-three minutes prior to obturation. I also like to use EDTA (ethylenediaminetetraacetic acid) intermittently to eliminate the smear layer and any nonorganic debris that have accumulated as a result of shaping and instrumenting the canal. The amount of irrigation that is used for both upper and lower is the same for a conventional root canal. In cases of retreatment irrigation is longer due to additional solutions used at the end prior to obturation.
6. Do you recommend crown lengthening before or after a root canal, and why?
In my opinion, the crown lengthening should be done after the root canal treatment has been completed. There are several reasons for this. One is that, in most cases, a root canal treatment determines the ultimate salvageability of the tooth and whether a proper restoration can be placed without compromising the integrity of the tooth. The second reason is the ease of treatment. Once crown lengthening is performed, due to the nature of the treatment and the amount of involvement with hard and soft tissues, it takes up to 10 weeks to achieve ideal healing before any additional stress—such as placing a rubber dam clamp on the tooth or having the patient stretch his or her cheeks open for long periods of time—can be applied to the tooth or surrounding structures. This type of delay in root canal treatment of a compromised tooth can potentially lead to complete failure of the tooth and further trauma from bacterial invasion or destruction of tooth structure under normal wear and tear. Another factor to consider is that by doing root canal treatment after crown lengthening, the newly formed Sharpey’s fibers and connective-tissue attachment can come under a tremendous amount of stress from the rubber dam clamp, especially in situations where there is no distal adjacent tooth to use as a clamp anchor. This type of stress can lead to further damage of the newly formed periodontal ligament (PDL) and connective tissues. (figure 3)
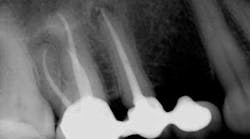
7. Why does some periapical pathology (PAP) last many years after the root canal treatment?
Some periapical radiolucencies (PARLs) (figure 4) may last up to five years after root canal treatment. One factor that contributes to the prolonged presence of PARLs is size of the initial lesion, such that larger lesions tend to last longer and heal at a slower rate. Location of the lesion is another factor that may contribute to this prolonged healing. Lesions in denser bone, such as the anterior mandible, tend to heal slower than lesions in less cortical bone, such as the posterior maxilla. The patient’s medical history is another factor that should be taken under consideration in such cases. Studies show that patients with diabetes, due to their lower immune system function, may require more time to heal. Some of the PAPs that tend to last can also be scar tissue in the bone.
8. How important is the access preparation, and what factor(s) play a role in a proper access preparation?
The entire root canal procedure is a series of steps that follow each other in a very logical order. If every step is done well, the final result will be achieved with ease and free of any stress. This process starts with a proper access cavity. Obtaining an ideal access is dependent upon several factors. The clinician’s knowledge of the anatomy of the pulp chamber, his or her experience in dealing with cases with unusual anatomies, the condition of the tooth prior to access (such as amount of intact tooth structure), the ability to obtain a straight line of access to each canal, and the location of the tooth in relation to other teeth are some of the most important factors that one must consider in order to achieve an ideal access.
Reference
1. Baumgartner JC, Xia T. Antibiotic susceptibility of bacteria associated with endodontic abscesses. J Endod. 2003;29(1):44–47.
Moji Bagheri, DMD, is an endodontist practicing in Orange County, California. He received his DMD in 2009 from Boston University’s Goldman School of Dental Medicine and his specialty training in endodontics from Rutgers University in 2014. He can be reached at [email protected].
Iman Sadri, DDS, is a cosmetic dentist and blogger practicing in Southern California. He received his DDS in 2008 from the New York University College of Dentistry. He can be reached at [email protected].
Originally posted in 2016 and updated regularly