The "new" periodontal disease: navigate the emerging solutions (Part 2)
Aug. 18, 2011
By Maria Perno Goldie, RDH, MS
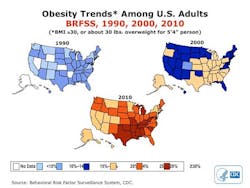
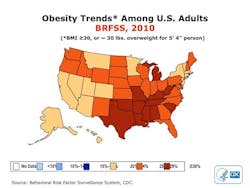
In this issue, we will continue our discussion of the link between systemic conditions and diseases and periodontal disease. We will explore the link between obesity, smoking ... on periodontal disease.Obesity, a marker of excessive fermentable carbohydrate intake, is associated with an increased risk of periodontal disease. (P. Hujoel. Dietary Carbohydrates and Dental-Systemic Diseases. J Dent Res 2009; 88; 490). In the United States, morbid obesity is increasing rapidly. One-third of the children born in 2000 are anticipated to develop diabetes in their lifetime. (Ezzati M, Friedman AB, Kulkarni SC, Murray CJ (2008). The reversal of fortunes: trends in county mortality and cross-county mortality disparities in the United States. PLoS Med 5(4):e66).
For the first time in decades, the life expectancy in large segments of the population is decreasing. Dental caries may be on the rise again in children. Obesity is on the rampage worldwide, as well. Its prevalence has tripled in many countries in the World Health Organization (WHO) European Region since the 1980s, and the numbers of those affected continue to rise at an alarming rate, particularly among children.
Obesity is already responsible for 2-8% of health costs and 10-13% of deaths in different parts of the Region. The World Health Organization estimating the numbers at more than 300 million worldwide, with a billion more overweight. It will increase health care cost and death rates around the globe. (www.who.int/mediacentre/factsheets/fs311/en/) With obesity comes the increased risk of: cardiovascular disease; type II diabetes; hypertension; and periodontal disease. (www.euro.who.int/document/E90711.pdf).
Chronic inflammation is a major cause of many degenerative diseases. One of the causes of chronic inflammation is obesity. Monocytes exist in a proinflammatory state in obese persons known to be at increased risk of developing diabetes, heart disease or both. Excess nutrients, such as fat and sugar, push some cells in the body over the brink. Unable to tolerate this “toxic” environment, these cells commit suicide. Under normal conditions. the small nucleolar RNAs involved with cell death are not activated and are not visible around the nuclei of these mouse muscle cells. In the presence of fats, however, the RNA molecules are activated and move out of the cell nuclei and into the cytoplasm, the liquid in the main body of the cell, where they help initiate cell death. This is the first time these small RNAs have been shown to function in the cytoplasm. (Carlos I. Michel, Christopher L. Holley, Benjamin S. Scruggs, Rohini Sidhu, Rita T. Brookheart, Laura L. Listenberger, Mark A. Behlke, Daniel S. Ory, Jean E. Schaffer. Small Nucleolar RNAs U32a, U33, and U35a Are Critical Mediators of Metabolic Stress. Cell:Volume 14, Issue 1: July 6, 2011, 33-44). There are three unexpected players in the mix. Small strands of RNA, a close chemical cousin to DNA, are critical mediators of oxidative stress and lipotoxicity. The research, published in the July 6, 2011 issue of Cell Metabolism, is the first to link these small RNA molecules to the cellular damage characteristic of common metabolic diseases like diabetes. Though cell suicide is a natural process that protects healthy tissues from damaged cells, it can sometimes fall out of balance. If the cell death pathway gets shut down, damaged cells may divide and lead to cancer. On the other hand, too much cell death due to abnormal metabolites, such as high levels of fats and sugar, can impair the function of tissues in the body. Such excess cell death is involved with diabetes complications such as heart failure. Understanding how abnormal metabolites cause cells to die will be helpful in the search for new therapies for these diseases.Both the emerging Randomized Controlled Clinical Trials (RCT) evidence and the ongoing obesity and diabetes epidemic may cause shifts in public health policies on dietary advice. Saturated fatty acids (SFAs) produce an inflammatory response in the body. Hyperinflammation is now recognized as one of the key underlying etiologic factors in periodontal disease. (M. Iwasaki, M.C. Manz, P. Moynihan, A. Yoshihara, K. Muramatsu, R. Watanabe, and H. Miyazaki. Relationship between Saturated Fatty Acids and Periodontal Disease. J Dent Res July 2011 90: 861-867.) The clinical relevance is that investigating the relationship between dietary SFAs and periodontal disease is important in understanding the potential role of dietary modification in periodontal disease intervention. It can ultimately help with prevention of periodontal-disease-associated tooth loss. Smoking has significant impact on the gingival and oropharyngeal flora. (I. Brook. The Impact of Smoking on Oral and Nasopharyngeal Bacterial Flora J Dent Res June 2011 90: 704-710.). The effects of exposure to smoking are apparent in both children and adults. Smoking increases the numbers of periodontal pathogens and periodontal disease, colonization by respiratory pathogens, and the occurrence of upper respiratory tract infections, including otitis media. The oral flora of smokers contains fewer aerobic and anaerobic organisms with interfering activity against bacterial pathogens and harbors more possible pathogens as compared with the flora of nonsmokers. The good news is that the high number of pathogens and the low number of interfering organisms found in the nasopharynx of smokers revert to normal levels after complete cessation of smoking. Parents who smoke harbor more latent pathogens and fewer interfering organisms, they may serve as a source of pathogens that can colonize and/or infect their children. The reduction in the number of members of the normal flora that interfere with the growth of pathogens and the greater adherence of bacterial pathogens to the oral mucosa are linked with a greater incidence of respiratory infections. Analysis of the data presented illustrates the adverse effects of direct and indirect exposure to smoking on colonization with potential pathogens.Smoking has a negative effect on bone regeneration following periodontal treatment. Patients should be advised that their smoking habit may result in poorer bone regeneration following periodontal treatment, based on six of ten studies in this review. (Rupal A. Patel, Ron F. Wilson, Richard M. Palmer. The Effect of Smoking on Periodontal Bone Regeneration: A Systematic Review and Meta-Analysis. Journal of Periodontology 31 May 2011: 1-18).Other issues discussed in this course related to women’s issues through the lifecycle, autoimmune diseases, and other conditions that could affect the periodontal condition. These will be discussed in future newsletters.
Maria Perno Goldie, RDH, MS
To read previous articles in RDH eVillage FOCUS from 2011 written by Maria Perno Goldie, go to articles.