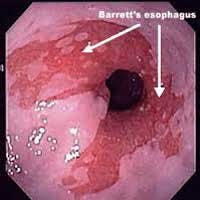
Barrett's esophagus to esophageal adenocarcinoma: Are you at risk?
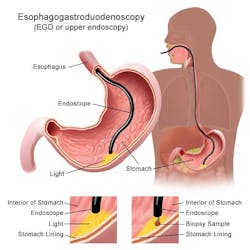
The risk of esophageal cancer in patients with Barrett’s esophagus is quite low, approximately 0.5 percent per year (or 1 out of 200). Therefore, the diagnosis of Barrett’s esophagus should not be a reason for alarm. It is, however, a reason for periodic endoscopies. If your initial biopsies don’t show dysplasia, endoscopy with biopsy should be repeated about every 3 years. If your biopsy shows dysplasia, your doctor will make further recommendations.
Esophageal cancer is the seventh leading cause of all deaths from cancer worldwide, with an estimated 14,000 deaths from this cancer in the United States alone in 2006. Since the 1970s, esophageal adenocarcinoma has been the neoplasm with the fastest-growing incidence of any cancer in the Western world.
This rising incidence implies a need for improvement in identifying those at risk for the disease and in both intervention and prevention. In the past, there has been a lack of consensus among experts regarding the diagnosis and management of Barrett's esophagus. Hopefully the new guidelines will assist practitioners in both prevention and intervention messages and strategies.
References
1. MedlinePlus. http://www.nlm.nih.gov/medlineplus/ency/article/000283.htm.
2. AACR in the News. Newly Identified Biomarkers May Help Predict Progression of Barrett's Esophagus to Esophageal Adenocarcinoma. Press release March 6, 2013. http://www.aacr.org/home/public--media/aacr-in-the-news.aspx?d=3028.
3. Wu X, Ajani JA, Gu1 J, Chang DW, Tan W, Hildebrandt MAT, Huang M, Wang KK, and Hawk E. MicroRNA Expression Signatures during Malignant Progression from Barrett's Esophagus to Esophageal Adenocarcinoma. Cancer Prev Res March 2013, 6; 196. doi: 10.1158/1940-6207.CAPR-12-0276.
4. 2009 Gastrointestinal Cancers Symposium (GICS): Abstract 2. Presented January 15, 2009.
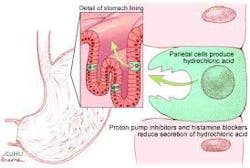
5. Katz PO, Gerson LB, and Vela MF. Guidelines for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol 2013; 108:308 – 328; doi: 10.1038/ajg.2012.444; published online 19 February 2013.
6. American Society for Gastrointestinal Endoscopy (ASGE). Patient Education brochure. http://www.asge.org/patients/patients.aspx?id=402.
7. Banerjee S and Van Dam J. GERD: Reflux to Esophageal Adenocarcinoma. N Engl J Med 2007; 356:1897-1898. May 3, 2007. DOI: 10.1056/NEJMbkrev57846.