The silent epidemic: How the dental profession overlooked the true culprit of TMJ disorders
For decades, the dental profession has grappled with temporomandibular joint (TMJ) disorders, a complex set of conditions affecting millions worldwide. Despite extensive research and clinical experience, a critical piece of the puzzle has remained elusive, leading to a narrow and often ineffective approach to diagnosis and treatment. This oversight has not only hindered progress in managing TMJ disorders but has led to potentially harmful interventions that fail to address the root causes of the problem.
While developmental deformities, osteoarthritis, and trauma play a role in TMD’s etiology, at the heart of this misconception lies the conflation of two powerful but distinct parafunctional activities: grinding and clenching. Both fall under the umbrella of bruxism, as defined by the American Academy of Orofacial Pain,1 yet they represent fundamentally different modes of force application to the TMJ.
Grinding has long been the focus of dental interventions, but it is clenching, now known as “dental compression syndrome” (DCS),2 that poses a far greater threat to joint health. The intense pressure from vertical forces, which are twice as powerful and last twice as long,3 not only surpasses the damage potential of grinding but stems from a broader range of etiological factors far beyond central nervous system triggers.
Yet the dental profession has largely ignored this critical distinction, instead focusing on occlusal adjustments4 and other interventions that primarily address the horizontal component of parafunction. While horizontal parafunction results in the condyle gliding past the discs with reduced impact, vertical parafunction forces the condyle to compress the disc, leading to microtrauma, inflammation, and eventual displacement. When disc displacement did occur, the dental community prioritized symptom management rather than preventive measures by replacing the damaged cartilage discs with Teflon-coated implants. This strategy exacerbated the condition resulting in the FDA’s recall of 25,000 implants,5 with one implant working its way into a patient’s brain. While clenching and grinding share certain central nervous system triggers, DCS has an extensive etiological portfolio that includes medications, exercise, sports, sleep apnea, pain, anger, fear, and stretching.2
Clenching doesn’t seem to bother most people as it works within one’s subconscious. So, when problems occur such as TMDs, damaged dentition, and alveolar bone loss, the focus is on the target, not on the source. Therefore, it is critical for the practitioner to recognize its signs. Unlike bruxism’s flattened dentition, DCS has a unique set of footprints; its signs and symptoms that qualify it as a syndrome were not identified and associated with compression until the early 1980s.6,7 Unlike bruxism, with which a guard will suffice while sleeping, DCS occurs while awake, requiring patients to monitor themselves. However, the practitioner must recognize its signs in order to alert the patient.
Hard tissue and prosthetic deformations due to DCS
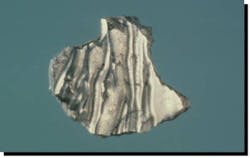
This unique loss of tooth structure (noncarious lesions, NCLs) has been the subject of controversy among dentists for almost 100 years (figure 1). W I Ferrier (1931) once remarked, “Their etiology seems to be shrouded in mystery.”8 We now understand that these multishaped deformations are examples of hard tissue fatigue due to compression failure. Fatigue, a weakened state brought about by repeated stressing, is one of the most insidious causes of loss of strength in a structure.9
Fatigue factors did not come into recognition until the introduction of rotating metal machinery in the middle of the nineteenth century. In time with the emerging science of biomechanics, dentists began to recognize their significance in the study of the mechanical behavior of living materials.10 Minute particles of tooth structure are being shed at vulnerable sites of high stress. The cuspid in figure 1 demonstrates changing sites of failure as alveolar bone recedes.
Another example is the formation of unique, highly polished, concavities at another focal point of high stress (figure 2). Kornfeld first observed this glassy sheen (1932) on both wedge-shaped NCLs and inverted cupolas.11 It is suggested that the glassy sheen is due to positive ions from the compression of apatite crystals, the piezoelectric effect.
Fatigue is easily recognized in prostheses and restorative materials (figures 3 and 4).
The wavy patterns in amalgam are termed Luder lines or slip bands due to molecules in the alloy rearranging themselves from compressive strain.
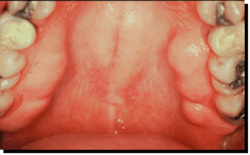
Contrarily, compression of alveolar bone results in additional bone (figures 5 and 6).
Articles on bony protrusions appeared in the literature as early as 1814.12 The negative ions generated from the compression of apatite crystals are believed to be responsible for the aggregates of new bone growth.2
Summary
A paradigm shift is necessary regarding TMDs. We have embraced and accommodated horizontal parafunction while ignoring clenching; it has been a critical oversight. A common inquiry asks the relationship of occlusion to TMDs: it would be better to question the liability of parafunction in the etiology of TMDs and then ask whether occlusion initiates the parafunction.
Since DCS can only be managed by the patient, the application of a small question mark on his/her cell phone is a helpful reminder.
Editor’s note: This article first appeared in Clinical Insights newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe.
References
- Okeson JP. Orofacial Pain: Guidelines for Assessment, Diagnosis and Management. Quintessence; 1996.
- McCoy G. Dental compression syndrome, a new look at an old disease. J Oral Implantol. 1999;25(1):35-49. doi:10.1563/1548-1336(1999)025<0035:DCSANL>2.3.CO;2
- Paesani DA. Bruxism, Theory and Practice. Quintessence Publishing Co.; 2010.
- McCoy G. The story of occlusion. J Oral Implantol. 2024;50(6):561-562. doi:10.1563/orim-50-6-editorial
- Wall Street Journal. August 31, 1993.
- McCoy G. The etiology of dental erosion. J Oral Implantol. 1982;10(3):361-362.
- McCoy G. On the longevity of teeth. J Oral Implantol. 1983;11(2):248-267.
- Ferrier WI. Clinical observations on erosions and their restorations. J Calif State Dent Assoc. 1931:187-196.
- Gordon JE. Structures or Why Things Don’t Fall Down. DaCapo Press; 1978:333-334.
- Gordon JE. The New Science of Structures and Materials. Scientific American Library; 1988.
- Kornfeld B. Preliminary report of clinical observation of cervical erosions. Dent Items of Interest. 1932;54(12):905-909.
- Sean TH. Torus palatinus and torus mandibularis: a review of the literature. Aust Dent J. 1995;40(5):318-321. doi:10.1111/j.1834-7819.1995.tb04820.x
About the Author
Gene McCoy, DDS
Gene McCoy, DDS, is an honored fellow with the American Academy of Implant Dentistry. Now retired, he has lectured Internationally and published extensively on occlusion and temporomandibular disorders. He can be contacted at [email protected].