As you can see, the 2012 IOM report recommended making schools a focal point for obesity prevention.(1) The development and implementation of K-12 nutrition curriculum benchmarks, guides, or standards would constitute a critical step in achieving this recommendation. On March 11-12, 2013, the IOM held a workshop to discuss the merits and potential uses of a set of national nutrition education curriculum standards and learning objectives for elementary and secondary school children. Workshop participants identified current promising practices, considered the most important attributes of such standards, and suggested approaches to build acceptance and use among educators. This document summarizes the workshop.(2) Nutrition education is a life skill that provides the appropriate knowledge and skills to eat healthfully, which affects both quality of life and longevity. Furthermore, research has shown that nutrition education can change behaviors.(2) Many questions remain regarding what should be taught, how it should be taught, and how much time needs to be devoted to nutrition education. However, there is ample evidence to convince people that nutrition education is effective. Poor nutrition continues to have an effect on bone health, as well as on dental health, which can affect eating, speaking, and attending to learning. Anorexia and bulimia are being seen in younger and younger children and in boys as well as girls. Night eating syndrome also is proving to be common in adults who eat large amounts of calories at night, and expose their children to this behavior. Many children in middle schools and even some in elementary schools are dieting. Changing behavior is more difficult than changing knowledge and behavioral change should be the goal of nutrition education. A meta-analysis of 12 meta-analyses found a positive effect on health behavior changes in eating and physical activity.(3) The task of this group was to discuss development of national nutrition education curriculum standards for use in elementary and secondary schools. The IOM as a whole has an extensive history of examining the nation’s nutritional well-being and providing sound information about food and nutrition. They work toward the safety and adequacy of the U.S. food supply, proper use of dietary supplements, the need for adequate nutrition among particular populations, and guidelines for nutrient intake.(4)Advancing Oral Health in America, a Consensus Report released April 8, 2011, discusses tooth decay and risk factors and preventive approaches for many oral diseases, and how oral health affects overall health and well-being.(5) Nutrition is integral to this process. As the baby boomers age, the population of Americans over the age of 65 is expected to increase to about 55 million in 2020, nearly 15 million more than in 2010. The increase in the older population will result in a surging demand for the delivery of services and create new challenges for older people, their caregivers, and nutrition and social services professionals who seek to ensure these services’ availability. Projections of an aging population with a greater chronic disease burden, as well as an increasing preference to live independently rather than in an institution, only add to the importance of preparation.
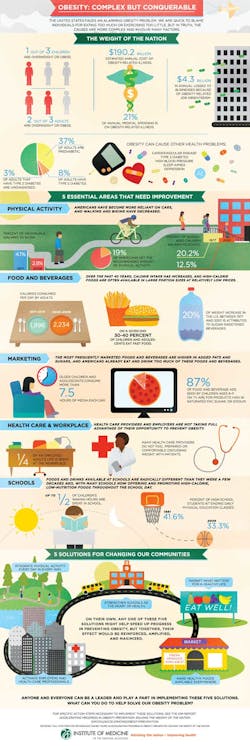
With approximately one-third of America’s youth overweight or obese, the childhood obesity epidemic and related health consequences are urgent public health problems. Health problems once seen mostly in adults, such as type 2 diabetes (formerly called adult diabetes), cardiovascular disease, and hypertension, are increasingly appearing in youth. Two-thirds of adults and one-third of children are overweight or obese. Left unchecked, obesity’s effects on health, health care costs, and our productivity as a nation could become catastrophic. The astounding human toll of obesity-related chronic disease and disability, and an annual cost of $190.2 billion for treating obesity-related illness, underscore the urgent need to strengthen prevention efforts in the United States.(1) The Robert Wood Johnson Foundation asked the Institute of Medicine (IOM) to identify catalysts that could speed progress in obesity prevention. The result is the 2012 IOM report, Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation.(1) The IOM evaluated prior obesity prevention strategies and identified recommendations to meet the following goals and accelerate progress. They are: integrate physical activity every day in every way; market what matters for a healthy life; make healthy foods and beverages available everywhere; activate employers and health care professionals; and strengthen schools as the heart of health. On their own, accomplishing any one of these might help speed up progress in preventing obesity, but together, their effects will be reinforced, amplified, and maximized.