Editor's note: Originally published October 31, 2017. Formatting updated November 15, 2022.
Presentation
A 60-year-old female with a noncontributory health history presented for a limited exam.
Chief complaint
The patient noticed some white tissue under her lower implant prosthesis (figure 1). She reported no pain in the area but was concerned about the tissue being something pathological. Apparently, when her implants were placed five years prior, a lesion of similar nature was removed and diagnosed as precancerous.
Three months earlier
The patient had been seen three months earlier for a recall exam and lower prosthesis removal and cleaning. Findings at the soft-tissue exam were within normal limits.
Clinical exam
Clinical assessment revealed a white, corrugated lesion lingual to the acrylic of the fixed hybrid prosthesis (figure 2). The lesion measured 5x24 mm and was not able to be scraped off or removed. It was not painful or symptomatic, and no swellings were noted in the sublingual or submandibular lymph node areas (figures 3 and 4).
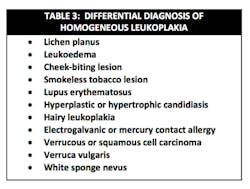
Differential diagnoses
- Squamous cell carcinoma
- Hyperkeratosis
- Localized lichen planus
Definitive diagnosis
Squamous mucosa with marked hyperkeratosis and no evidence of malignancy or dysplasia
Follow-up and treatment
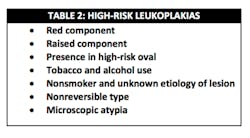
The unknown etiology of the lesion automatically put it into a category of high-risk leukoplakia, especially since it had just recently manifested and there had been a history of previous biopsy to the area that was diagnosed as precancerous tissue. The patient was seen in my office for prosthesis removal and then referred to an oral surgeon, where she had an excisional biopsy under local anesthesia (figures 5 and 6). The patient's prosthesis was adjusted and appropriate follow-up care was put in place.
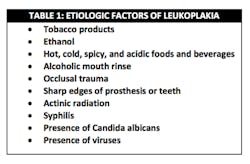
Discussion and study: Leukoplakic lesions
Hyperkeratosis is defined as an “excessively thickened layer of the stratum corneum composed of orthokeratin (hyperorthokeratosis) or parakeratin (hyperparakeratosis).”1 The majority of leukoplakias are hyperkeratoses.1 Keratin functions as a protective barrier on normal mucosa or skin; if stimulated, additional keratin layers are formed.1 These stimuli include ill-fitting dentures and smoking/smokeless tobacco.
Take a look at this case: A patient with a leukoplakic lesion and a noncontributory health history. The following is taken from that case and gives a general background on leukoplakic lesions.
"The presence of leukoplakic lesions in the oral cavity is always cause for evaluation and follow-up. The World Health Organization defines leukoplakia as “a white patch or plaque that cannot be characterized clinically or pathologically as any other disease.”2 Leukoplakic lesions are one of the more common forms of epithelial dysplasia, typically discovered during routine exams; they are usually asymptomatic and represent 6.2% of all oral biopsy specimens.2 Leukoplakia and squamous cell carcinoma (SCC) share many of the same etiology factors,2 and approximately 5.4% of leukoplakic lesions become SCC.1 It is, therefore, imperative that the following steps be considered:2
General reminders with regard to squamous cell carcinoma1
- Malignant neoplasm of stratified squamous epithelium is capable of locally destructive growth and distant metastasis
- Represents 3% of all cancer in males and 2% in females; overall survival rate with patients who have oral malignancies is 50%
- Represents 90% of all oral cancers and is by far the most common malignant neoplasm of the oral cavity
- Occurs in various sites but most commonly found on the lower lip, lateral boarders of the tongue, and the floor of the mouth.
- Etiologic factors include tobacco, alcohol consumption, viruses, radiation, immunosuppression, nutritional deficiencies, preexisting diseases, and chronic irritation.
- Has a number of different clinical presentations, most commonly presenting as leukoplakias and erythroplakias.
References
- Sapp JP, Eversole LR, Wysocki GP. Contemporary Oral and Maxillofacial Pathology. St. Louis, MO: Mosby; 1997.
- Wood NK, Goaz PW. Differential Diagnosis of Oral and Maxillofacial Lesions. 5th ed. St. Louis, MO: Mosby; 1997:75-77, 98-103, 106-107.