Jaw and muscle strain/sprain, sometimes called JAMSS, is a localized acute musculoskeletal disorder that can result from a traumatic or mechanical injury. It can cause sudden jaw pain, limited range of motion, tenderness, or dysfunction. Trauma to the jaw includes a direct blow, previous injuries, bruxism (clenching/grinding), yawning too wide, taking a big bite of food, lengthy dental appointments, or dental injections. If any of these have happened, you could be at a higher risk for jaw joint and muscle strain/sprain.
Sprain is the excessive stretching or tearing of ligaments. Jaw sprain can happen to the ligaments surrounding the jaw when they are stretched further than normal. The tearing of the ligament fibers varies from mild to severe depending on the number of ligaments torn.
Strain involves an injury to the muscle or tendons. Strains particularly to the jaw happen due to the constraints and demands placed on the muscle fibers. If the muscles can’t handle the stress, it can cause the muscle fibers to tear.1
Common signs and symptoms
- Jaw pain or tenderness
- Jaw popping or trismus
- Cheek muscle tightness or stiffness
- Head or earaches
- Limited range of jaw movement
- Difficulty or pain when opening the mouth wide (or at all)
- Pain when chewing or biting
- Had recent dental treatment
- A feeling of hesitation or twinge when the mouth is open wider than it should, and your hand immediately moves to the jaw as if to comfort or support it
- A feeling that your jaw requires caution or “babying” when you close your mouth
Are you at moderate to higher risk?
Moderate to higher risk patients often have had previous jaw issues. If you’re a patient with a higher risk level for jaw muscle strain/sprain, be aware of dental appointments that can make the situation more likely.
Common conditions for sprain/strain include:
- long appointments
- multiple appointments in a short time frame
- multiple injections
- bilateral work in the back teeth.
If you have jaw pain after an appointment, consider these factors.
Many times, post-op pain is shrugged off as an expected part of dental treatment. That can be true, but if it lasts more than a week it’s beyond the normal pain level of a dental procedure. It’s important to treat jaw sprain and strain as soon as possible to keep it from becoming chronic and lasting. In a study from the Journal of American Dental Association, 61% of jaw trauma cases came from dental treatment, with 23% of these cases from new-onset trauma from third molar extractions.2
Jaw joint and muscle strain/sprain is a common outcome of wisdom teeth extractions. These procedures are bilateral, multiple injections that include the lower arch, which are at a higher risk for nerve, blood vessels, and tissue trauma. This is a procedure where the mouth needs to be opened wide, easily overextending the ligaments, tendons, and muscles. Another characteristic of this dental procedure is an abundance of pressure or force that may be needed to remove the teeth, especially if the teeth are significantly in the bone or have long roots anchored in pretty well. If the procedure takes longer and it’s painful to keep the mouth open (and just as unbearable to close it), you may be experiencing jaw joint and muscle strain/sprain. When you’re at the breaking point and the procedure isn’t quite done, it’s common to get reassurance from the dental professional that “we’re almost done, hang in there”—you may be experiencing the perfect storm of jaw joint and muscle strain/sprain.
If you have jaw pain from any cause but especially from previous dental appointments, be aware that there are options to mitigate some pain.
Treatment for jaw joint and muscle strain/sprain
Sprain and strains may affect different people differently, but the causes, symptoms, and treatments are the same.
- During a dental procedure, don’t be afraid to ask for breaks; as well, a bite block will help lessen the strain on the muscles as they to stay open.
- You should also take an anti-inflammatory prior to treatment.
- Some days are better than others, and that relates to what the body can handle or not on a given day.
- If keeping your mouth open is excruciating the day of the appointment and rescheduling or stopping halfway through is absolutely necessary, communicate with the dentist.
- Ask for shorter appointment times where one or two fillings will be completed at a sitting rather than five or more.
- Ask for breaks during the treatment, and if you know you’re a significant risk for jaw joint and muscle strain/sprain, let the dental office know so the appointment can be scheduled appropriately with added time for breaks. The goal for you is not to feel debilitated after a procedure to the point where you are unable to open or eat afterward.
Post-treatment recommendations
Medication: Use NSAIDS or aspirin as an anti-inflammatory and pain reducing apparatuses.
Cold and heat compresses: When a strain happens in the muscles, fibers in the tissue are damaged to cause immediate pain, inflammation, and swelling. Apply cold on the tender area to reduce the inflammation as soon as possible. While cold relieves pain after the initial swelling has decreased, heat increases oxygen supply which carries nutrients to the damaged tissue to promote healing.
Applying pressure helps remove excess fluid and cellular waste and improves range of motion. It helps loosen tight muscles and increases blood flow to help heal damaged tissues.
Massage helps reduce swelling and inflammation as those factors intensify pain and slow healing, and it promotes good blood circulation.
Eating: Chew on both sides of the mouth to even out pressure, and stick to softer foods.
Avoid damaging habits: The following can cause undue stress and pressure on the jaw: bruxism; clenching; biting your cheeks, tongue, and lips; resting the jaw on the hand; and opening mouth too wide or too long.
Jaw exercises: Exercises improve the tightness in the jaw and muscles to restore function and range of motion. Place the tongue behind the top middle front teeth and open the mouth as comfortably wide as possible and then close. Perform for 10 counts about three times a day for at least one week.3
If there is limited and rigid range to opening, place two fingers horizontally between the front teeth and hold to a count of 10; gradually make that to three fingers.
Using a splint
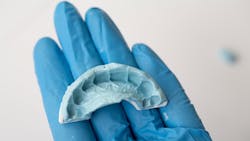
If you’re at a higher risk for jaw joint and muscle strain/sprain and orofacial pain during or after treatment, ask the dentist about an immediate prefabricated anterior bite splint called Quicksplint (see figures 1 and 2). It is a relined splint for a custom fit that can be fitted the day of treatment. It’s engineered as an anterior deprogrammer for quicker recovery and to wear at night and reduce oral habits, allowing the jaw muscles and joints to relax and rest and heal more quickly.4
This type of splint is not only beneficial for a limited time after treatment for jaw joint and muscle strain/sprain, but it’s also helpful for when you eventually need a night guard. Using Quicksplint until your treatment is fully completed and all work is done will protect your teeth until you can get a nightguard.
The most important takeaway is to get treatment right away if your jaw is sore more than a few days after a dental procedure. Jaw pain shouldn’t last for more than a week after treatment. Studies show that getting pain resolved quickly can help prevent long-term jaw pain and promote quicker healing. If jaw pain is treated within a week, the chances of it healing successfully within four weeks is much greater. Patients who haven’t been treated early have reported pain years after the initial injury.
Jaw joint and muscle strain/sprain isn’t uncommon but it’s often underreported, misdiagnosed, and misunderstood. Many dental professionals may not relate this condition to dental procedures—but when jaw injury happens, no matter how it happens, it should be treated swiftly and consistently. If jaw joint and muscle strain/sprain does happen in the dental chair, knowing the symptoms and treatments (before and after) can help tremendously with recovery and healing.
References
1. What is jaw strain or motion? Pivotal motion. https://pivotalmotion.physio/jaw-strain-sprain/
2. Fricton J, Eli B, Gupta A, Johnson N, DDS, PhD. Preventing chronic pain after acute jaw sprain or strain. J American Dental Association. https://jada.ada.org/article/S0002-8177(16)30569-4/fulltext
3. Jaw Rx-ercises: Therapeutic techniques to relax jaw muscles. https://cdn.shopify.com/s/files/1/0058/4128/9314/files/Jaw_Rx-Ercises.pdf?v=1600712903
4. Eli B, Fricton J. Jaw joint and muscle strain/sprain treatment technique. Oral Health. July 11, 2016. https://www.oralhealthgroup.com/features/jaw-joint-muscle-strainsprain-treatment-technique/
About the Author

Lara James, RDH
Lara James, RDH, is a licensed dental hygienist with more than 15-plus years of clinical hygiene experience in corporate, dental management, and private practices. She has created DentalAisle.com, a dental blog to educate consumers on dental products and dental issues. Lara also has written an online continuing education course on dentalcare.com. For more information, email her at [email protected].
Updated October 26, 2022