Case presentation and medical history
A 60-year-old female presents for a new patient exam to “get established.” She had no concerns. Medical history, other than occasional social smoking and acetaminophen allergy, was insignificant. Dental history, however, was not so vanilla.
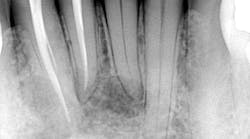
Approximately five years ago, at one of her general dental appointments, she had informed her dentist that she had some tenderness in the proximity of her lower front jaw. Radiographic assessment had apparently revealed numerous radiolucent lesions in the anterior mandibular area. The patient was referred to an oral surgeon, who removed the lesions and sent them off for biopsy. The definitive diagnosis was glandular odontogenic cyst. Postsurgery, it was recommended that the patient be diligent with her recare exams, specifically radiographic follow-up as the lesions tend to recur.
Clinical exam
At her visit with me, the updated radiographs showed the presence of multilocular radiolucencies in the lower anterior area.Some tenderness was present but vague and very sporadic. Since there was a history to the area, it warranted another assessment and biopsy. As a side note, teeth nos. 25 and 26 had root canals on them, which I suspect were done because of the radiolucencies in the area. All other lower anterior teeth tested vital.
Diagnosis and discussion
The patient was referred to an oral surgeon who performed curettage on the lesions and sent the tissue off to pathology. This was the attending pathologist’s report:
“…based on the morphology, I favor lateral periodontal cyst, although recurrences are more typical of the polycystic variant termed botryoid odontogenic cyst. I note that there is a reported ‘history of glandular odontogenic cyst in the same location,’ highlighting the well-known challenge differentiating lateral periodontal cyst from glandular odontogenic cyst…both lateral periodontal cyst and odontogenic keratocyst are believed to be derived from dental lamina. Clinical follow-up is recommended to ensure resolution of the radiographic abnormality.”
So, there’s a flip-flop diagnosis between the patient’s original lesion and the current lesion, both of which have a similar origin. Here is some basic information about lateral periodontal cysts and glandular odontogenic cysts.
Lateral periodontal cyst (aka botryoid odontogenic cyst)1
- Slow-growing, no expansile developmental odontogenic cyst derived from one or more tests of the dental lamina
- Shares numerous clinical and morphologic similarities with the gingival cyst of the adult
- Typically seen as well-defined, delicately corticated, solitary radiolucency located between the roots of vital teeth, usually less than 1 cm in diameter
- Most commonly found in the premolar region with occasional appearances in the anterior maxilla and mandibular areas
- Mean age is 50 years old
- Recurrence is uncommon after surgical enucleation
Glandular odontogenic cyst (aka sialo-odontogenic cyst)1
- Unusually large solitary or multilocular odontogenic cyst, primarily in the mandible
- Greater growth potential than lateral periodontal cyst and a propensity to recur
- Nonspecific radiographic appearance, with lesions commonly large, well-defined, and with unilocular or multilocular radiolucencies
- Treatment is surgical enucleation and curettage
It would seem, given the patient’s history and the general description of the lesions, that this recurrence would likely be diagnosed as a glandular odontogenic cyst. However, it could very well be that it was indeed one lesion, and then later on exhibited the other specifics of the pathology reports. Is that bad? No, because regardless, we can conclude from either diagnosis that there is no threatening pathology; treatment for both lesions is the same and patient outcome is favorable. This patient has been placed on a regular recall regimen with routine radiographic assessments.
Editor’s note: This article first appeared in Through the Loupes newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe to Through the Loupes.
Reference
- Sapp JP. Eversole LR, Wysocki GP. Contemporary Oral and Maxillofacial Pathology. Mosby; 1997:48-51.