There’s more to drug-induced dry mouth than you think
Here’s a sobering thought: In 2020, it’s estimated that 4.55 billion prescriptions will be filled in the United States.1 Yes. Billion. While the need for these medications is not up for debate (although it certainly is a topic worthy of a candid discussion), their use and subsequent systemic side effects are definitely present. With regard to oral health, these side effects often come in the form of hyposalivation (decreased saliva production) and xerostomia (feeling of dry mouth), which leave the patient susceptible to a host of additional complications.
Dry mouth can lead to several oral health concerns such as difficulty swallowing foods, taste alteration, burning, and soreness. Progression will see the filiform papillae on the tongue atrophy in addition to a generalized erythematous mucosa. Additionally, a change in oral flora is common, resulting in an infection of Candida albicans, aka thrush.2 Buffering of oral acids and the capacity to inhibit cariogenic microorganisms are diminished, subsequently leading to the development of generalized rampant caries in the cervical area.2,3 These medications can seriously alter a patient’s way of life.
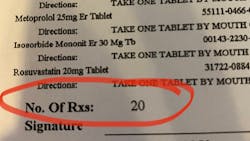
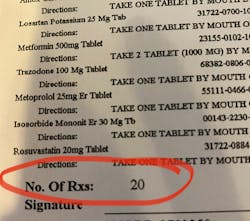
While there are nonpharmacologic causes of dry mouth such as trauma, autoimmune diseases, endocrine disorders, hyposecretory conditions, mental illness, and radiation treatment,3 the nation’s growing geriatric population will require increasingly complex pharmacologic management of multiple disease states such as cancer, hypertension, congestive heart failure, diabetes, arthritis, and osteoporosis.2 As said management unfolds, patients find themselves on a cocktail of medications that exacerbate dry mouth. These medications range in use and severity and may surprise you, as several of them are common everyday scripts and over-the-counter drugs. Take a look at this list of xerostomia-causing medications.4
Case report
Upon receiving approval from his oncologist to commence with dental care three months later, his examination revealed the following (figures 1-5):
- Severe class III active periodontal disease
- Rampant, generalized cervical caries with some lesions quite extensive in nature
- Broken no. 8 (chief complaint)
- Broken/carious nos. 18, 19, and 30; caries on no. 2
- Generalized dry mouth with white patchy mucosa; he did have a complaint of having a “sticky mouth.” Note: When we took the photos, we had to put water in his mouth because it was so dry.
The genesis for his caries was evident–drug-induced dry mouth and time were the perfect storm for widespread infection that demanded immediate management. Suffice to say, my news to the patient was not welcome.
Treatment for these types of patients is twofold in that the cause and effect are both parts of the problem-solving equation. Management includes palliative, saliva substitutes/lubricants, and cholinergic salivary stimulants. Each has pros and cons, and the patient may or may not get relief that is long term or ideal, and therein lies the challenge. Having an open dialogue and educating the patient while keeping the physician in the loop is advised, as sometimes medications can be switched or altered in frequency, etc.
Dry mouth products
Here’s a list of product suggestions to consider:2,3
Saliva substitutes/oral lubricants
- Prescription: Aquoral, Caphosol, Numoisyn
- OTC: Entertainer’s Secret, Moi-Stir, MouthKote, NeutraSal, Salese, Saliva Substitute, Salivert, SalivaSure
OTC saliva stimulants, primarily gum/lozenges
- Xylifresh, Biotène, Salix Lozenges
Prescription/cholinergic salivary stimulants
- Pilocarpine, cevimeline
Interestingly, as I’m finishing this write-up, I just did a limited exam on a 55-year-old patient who couldn’t remember her complete medication list. The pharmacy faxed it over; it was 20 deep and several of those were xerostomia-causing drugs (figure 6). I’m sure you can guess the rest of the story…
References
- Shahbandeh M. Total number of retail prescriptions filled annually in the United States from 2013 to 2025 (in billions). Nov. 12, 2019. https://www.statista.com/statistics/261303/total-number-of-retail-prescriptions-filled-annually-in-the-us/. Accessed Jul. 12, 2020.
- Moore PA, Guttenheimer J. Medication-induced hyposalivation: etiology, diagnosis, and treatment. Compendium. 2008;20(1):50-55.
- Bartok V. Drug-induced dry mouth. Pharmacy Times. November 9, 2011. https://www.pharmacytimes.com/publications/issue/2011/November2011/Drug-Induced-Dry-Mouth
- Medications that may cause dry mouth. Oral BioTech. http://wsdha.com/clientuploads/pdfs/Public%20Info/Seniors/DryMouthMedications.pdf. Accessed Jul. 12, 2020.
About the Author
Stacey L. Gividen, DDS
Stacey L. Gividen, DDS, a graduate of Marquette University School of Dentistry, is in private practice in Montana. She is a guest lecturer at the University of Montana in the Anatomy and Physiology Department. Dr. Gividen has contributed to DentistryIQ, Perio-Implant Advisory, and Dental Economics. You may contact her at [email protected].