How to prevent root resorption using the Golden Rule of Orthodontics
Editor’s note: There is nothing worse than telling patients in ortho they are going to lose their tooth due to root resorption, because what you say and what they hear are two different things. "My body is eating my tooth?!" Can this be prevented? The answer is yes, by following the Golden Rule of Orthodontics.
As chief of orthodontics at NYU Lutheran Pediatric Dental Residency and at Rady Children’s Hospital–San Diego, I regularly provide didactic and clinical instruction to nonorthodontic residents. I find that orthodontics is a topic that most of my residents are eager to learn about. I structure this education so that the learning experience will be rewarding rather than punishing, so with that in mind, I begin instruction for each new class of residents with the Golden Rule of Orthodontics: Primum non nocere.
While not specifically in the Hippocratic Oath, primum non nocere is believed to be derived from it and means first, do no harm or above all else, do no harm. In other words, before you do anything to a patient, make sure that you are not making matters worse. What good does it do to straighten teeth if in doing so you cause the patient to lose them? The point of this article is not to scare or deter you from engaging in orthodontics, but to give you a foundation that will protect both you and the patient.
ADDITIONAL READING | Orthodontic case study using the Differential Straight-Arch Technique yields remarkable results without surgery, extractions, or headgear
What is the worst thing that could happen? The answer, of course, is death. While treatment may have gone horribly awry, if your patient dies due to orthodontic treatment, that is the worst possible outcome. Always make sure to check the medical history.
Other than death, what will cause an orthodontist to lose sleep? Four things top the list:
- Root resorption
- White spot lesions (also known as decalcification)
- Periodontal disease
- Moving teeth out of bone
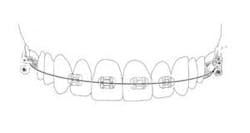
Before you begin treatment, take records. These include photos, x-rays, and diagnostic models. It is important to document the state of the patient prior to treatment. Regarding root resorption, it is essential to take radiographs. Any orthodontic treatment should include pretreatment and post-treatment radiographs that allow visualization of the roots. I recommend panoramic radiographs for this purpose. While it is common in general dentistry to take panoramic x-rays every five years, this is too long for patients in orthodontic treatment. Root resorption can be evident radiographically in as little as six months of orthodontic treatment. Because of this, I take panoramic x-rays every six to eight months in my practice.
ADDITIONAL READING | Maxillary expansion or bicuspid extraction: A case study in orthodontics
ADDITIONAL READING | Periodontally accelerated osteogenic orthodontics reduces treatment times in comprehensive orthodontic cases
Some evidence exists that stopping orthodontic tooth movement for six months or more will minimize root resorption if treatment is reinitiated. However, this is not conclusive, and there is no guarantee that such a protocol will work. Any decision to reinitiate should probably be made by an orthodontist.
Providing orthodontic treatment can be a very rewarding experience, when performed properly. Proper treatment requires planning. The safety of the patient is of paramount importance and the foundation upon which a good treatment plan is built. Always remember the Golden Rule of Orthodontics: Do no harm.
Editor’s note: This article appeared in Chairside Daily newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles at this link and subscribe here.
Joseph Morneau, DDS, is a 2001 graduate from Louisiana State University School of Dentistry. He received his orthodontic specialty certificate from St. Barnabas Hospital in New York. He is a veteran of the US Navy and has served as a dental officer in Italy, Japan, the Middle East, and California. It was during this time that he realized his passion for orthodontics. He now practices full time as an orthodontist in private practice in San Marcos, California. Dr. Morneau is also chief of orthodontics at NYU Lutheran Pediatric Dental Residency and at Rady Children’s Hospital–San Diego. He likes spending time with his beautiful wife, Vera, and their happy and healthy son, Hugo. He also enjoys surfing and travel in his spare time.