Each year, dental and dental hygiene students are taught the skill of performing an extraoral/intraoral (eo/io) cancer screening. The goal of this procedure is to discern abnormal from atypical.
While not all atypical findings are pathological, it is prudent that all findings be documented and followed. Lesions should be described in terms of color, size, texture, duration, pain, etc. and potentially, photographed for baseline data. For suspicious cases, a referral to a specialist is warranted immediately.
During the 2018-2019 academic year, there were 25,381 students enrolled in predoctoral dental education programs.1 Furthermore, there are 327 entry-level dental hygiene programs, approximately 51 degree-completion programs in dental hygiene (bachelor) and 17 master’s degree programs in dental hygiene.2
With so many practitioners possessing this invaluable skillset, why are patients frequently surprised when an astute care provider performs this service? Are we not providing this level of care due to time constraints, lack of reimbursement, or possibly, provider insecurity/lack of confidence? Studies of the comprehensiveness of exams reveal that many providers are not performing the exam in its entirety, if at all.3 The “option” to offer this service each and every visit should not be optional at all.
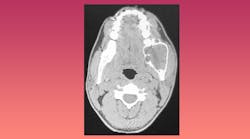
A case was documented at a dental school in which a former dental hygienist, now a second-year dental student, palpated what she perceived to be an anomaly in the mandible of a 68-year-old male. The patient had a history of ameloblastoma in 2013. An ameloblastoma is a benign odontogenic tumor generally present in the jawbone.4 He had been asymptomatic for approximately 2 years.
Presenting in 2019, the student dentist felt that a follow-up CT should be obtained. At that time, it was determined that recurrence was possible, and a series of referrals and images were initiated. By January 2020, a second surgery had been performed and the patient was reported to be doing well. This, and cases similar are the justification for an EO/IO at every visit, as even some benign lesions have the potential to metastasize or redevelop more aggressively.
Cases such as this are not rare. According to the American Cancer Society, oral cavity and oropharyngeal cancers occur most often on the tongue, the tonsils and oropharynx, and the gums, floor of the mouth, and other parts of the mouth.5 American Cancer Society’s most recent estimates for oral cavity and oropharyngeal cancers in the United States for 2021 are that about 54,000 people will develop these diseases, and about 11,000 will die as a result.5
Dental and dental hygiene students have a moral and ethical responsibility to treat the entire patient. This is referred to as Whole Person Health-care. Patients should be assured that a trained professional is observing, palpating, and documenting all structures associated with the oral cavity and head and neck region. To neglect this responsibility is neither acceptable nor professional.
How can we, as dental care providers, not only provide this service to each patient, every visit, but share with patients how to conduct their own brief oral cancer screening?
Most patients are aware that smoking is a significant contributor to oral cancer, but it is not the only factor. We also evaluate the surface of the skin. As a care provider, patients should be informed that an annual dermatology visit is suggested to evaluate any lesion, suspect or not, for skin cancer. Patients should also be advised to utilize sunscreen and lip protection with SPF.
Part of your intraoral and extraoral exam should be to allow the patient to observe what you are observing and explaining what you are looking for. Examples of conditions that might warrant further investigation or questioning might include:
- A sore in the mouth that does not resolve within two weeks (is there a history of pizza palate burn or taco chip trauma?)
- Any swelling in the tissues
- Unusual bleeding in the mouth
- Lymph nodes that appear to be swollen (without recent history of illness)
- Red or white areas in the mouth
- Teeth that are mobile (not associated with a history of dental disease)
- Sores on the skin that do not appear to be healing
Patients should be shown how to move their tongue from side to side, feel for lymph nodes, view the ventral portion of the tongue, and floor of the mouth. This is especially true for patients who smoke and/or chew tobacco.
While these findings are not definitive for oral cancer, there should be no delay in referral to a specialist.
How you present these findings to your patient is also critical. It is imperative to use verbiage that is both straightforward yet not overly alarming. If you are making a referral, patients are astute enough to understand there is need for concern. If they ask if they have oral cancer, perhaps the best response is to explain that there are a myriad of possibilities and that microscopic evaluation is the only way to know what is causing the condition and the best course of treatment. In many cases, the lesion biopsy results are benign, and all parties involved can breathe a sigh of relief. Improper verbiage, such as, “I’m sending you to the oral surgeon so they can see if you have cancer” only serves to increase anxiety and fear. If the results are not what we hoped for, we can address those fears at that time.6
Remember, you are looked upon as the expert. Explain to them that we conduct these exams and make referrals out of an abundance of caution, but we do suggest they have it addressed so that anything more serious can be ruled out.
Also keep in mind that a large segment of the population is not medically literate so keep your verbiage and jargon at a level they will comprehend. Words like lesion, biopsy, gingival bleeding etc. are likely to be unfamiliar. If they do not understand that bleeding gums is the same as gingival bleeding, they may not report that they have experienced an unusual amount of bleeding and therefore, lead you to believe that this condition is not present.6
If you practice long enough, I believe you will save a life! You may never know if the patient you referred was diagnosed and successfully treated due to your diligence and professionalism. Every patient, every visit should be part of your office vision and mission statement and every patient should know what you are doing and why you are doing it. You should stress that your office promotes whole body care and while teeth are your focus, as dentists, dental hygienists, and dental assistants, you also integrate all other body organ functions by thoroughly reviewing their health history at each visit (correlating systemic disease with oral conditions) and evaluating all eo/io structures.
With this care model, I assure you that you will sleep better each night knowing that you did the absolute best you can in treating your patients and it will set you apart from “drill and fill” offices.
This will be the best marketing you can have, and it will not cost you a dime!
References- Clinical resources: Education. American Dental Association Health Policy Institute. https://www.ada.org/en/science-research/health-policy-institute/dental-statistics/education#:~:text=How%20many%20dental%20schools%20are
- Dental hygiene by the numbers. American Dental Education Association. https://www.adea.org/GoDental/Future_Dental_Hygienists/Dental_hygiene_by_the_numbers.aspx
- Tax CL, Haslam SK, Brillant M, Doucette HJ, Cameron JE, Wade SE. Oral cancer screening: knowledge is not enough. Int J Dent Hyg. 2017 Aug;15(3):179-186. doi:10.1111/idh.12172
- Masthan KM, Anitha N, Krupaa J, Manikkam S. Ameloblastoma. J Pharm Bioallied Sci. 2015 Apr;7(Suppl 1):S167-70. doi:10.4103/0975-7406.155891
- Key statistics for oral cavity and oropharyngeal cancers. American Cancer Society. https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html
- Paz D. Did they really just say that? RDH magazine. December 1, 2011. https://www.rdhmag.com/patient-care/radiology/article/16408631/did-they-really-just-say-that