TMD-airway connection: The importance of dental and medical screenings
There’s a lot of discussion going on regarding the relationship between temporomandibular disorders (TMD) and airway disorders. Many dentists look for TMJ issues or problems with a patient’s bite, but oftentimes the cause of a patient’s issues may be related to airway and breathing complications. Therefore, signs and symptoms must be evaluated and identified through airway and medical screenings.
For example, allergies, deviated septum, upper airway inflammation and infection, and deformation can all cause airway obstruction and difficulty in nasal breathing. Strong evidence shows these obstructions can convert normal nasal breathing to mouth breathing.
Mouth breathing bypasses a person’s normal physiologic filtration system through the nose. Breathing dirty air through the mouth can be a source of inflammation and infection in the posterior throat and tonsil area. It can result in swollen tonsils and difficulty breathing through both the nose and mouth, and it can induce problematic ventilation during sleep. In turn, it can lead to both upper airway resistance syndrome (UARS) and, in more severe cases, obstructive sleep apnea (OSA).
With such potentially serious medical issues and complications, it is very important for all dentists to screen every patient for breathing and airway concerns.
Signs and symptoms during medical screenings
A few months ago, a dentist named Danny traveled from Sydney, Australia, to St. Petersburg, Florida, to attend one of The Dawson Academy’s courses. Danny was only in town for a few days, but he was experiencing some problems that he thought I could help solve. I agreed to see him as a patient, so we met to discuss his issues, take photographs, and complete a new-patient exam, which includes airway and medical screenings (figure 1).
Figure 1: Danny
Danny shared that he’d been experiencing problems that he felt might require a bite adjustment or possibly orthodontic correction.
His chief complaints were:
- Frequent morning headaches
- Clenching both day and night
- Chronically sore jaw and neck muscles
- Joint clicking on the left side
- Bite relationship feels off
- Teeth crowding
- Slight wear on the anterior teeth
- Chronic use of nasal decongestants
Another dental office might have identified Danny as a classic patient with TMJ and bite issues. However, many of these symptoms—such as frequent headaches, clenching, sore jaw, and crowded teeth—are also common indicators of airway issues. Through screens for airway and breathing disorders, we were able to identify these signs and symptoms as red flags for airway issues (figures 2–4).
Figures 2 and 3: Crowding of the lower anterior teeth and scalloping of the tongue. These are common findings with airway and breathing disorders.
Figure 4: Maxillary and mandibular retrusion.
Systematic approach to evaluating airway issues
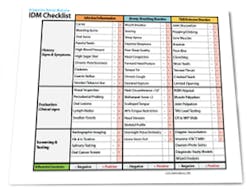
It is helpful for time-savings and accuracy to have a systematic approach for evaluating patients who may present with symptoms of potentially overlapping disorders. As we evaluated Danny’s complex presentation, we used the Integrative Dental Medicine (IDM) checklist as a guide (figure 5). This checklist evaluates three aspects of the patient: infection/inflammation, airway/breathing, and TMD/occlusion. These three areas are evaluated through a history of signs and symptoms, evaluation of clinical signs, and, finally, screening and testing.
Figure 6: Extremely enlarged tonsillar tissue obstructing the posterior airway
Figure 7: Ankyloglossia—75% tongue-tie constriction
Figure 8: Deviated nasal septum and narrowed airway
Figure 9: 95% obstructed posterior airway due to extremely enlarged tonsils
Positive signs/symptoms for TMD and occlusal issues:
- Joint discomfort
- Popping/clicking
- Sore muscles
- Bruxism
- Poor bite
- Clenching
- Worn teeth
- Crooked teeth
- Limited opening
After we reviewed Danny’s history of signs and symptoms, we began to evaluate the clinical signs for the three areas, which indicated the following.
Clinical signs for infection and inflammation:
- Swollen tonsils
Clinical signs for airway and breathing:
- Mallampati score greater than two
- Scalloped tongue
- 75% tongue restriction
Clinical signs for TMD and occlusion:
- Muscle palpation/tenderness
- Occlusal slide from centric relation to maximum intercuspation position with inadequate anterior guidance
Screening, testing, and findings
After identifying Danny’s history and evaluating the clinical signs, we moved to screening and testing. We recommended a home sleep test for his airway and breathing problems, as well as a Doppler auscultation and CBCT imaging for the TMD and occlusal issues.
The Doppler auscultation revealed reciprocal click on the left temporomandibular joint. The CBCT revealed normal joint anatomy, nasal airway obstruction with a slight deviated septum, and approximately 95% tonsillar obstruction in the posterior throat region. These findings led us to the conclusion of a positive airway/breathing disorder, with a Piper Stage I right temporomandibular joint and Piper Stage IIIa left temporomandibular joint.
We began to develop medical priorities based on the information gathered through the history of signs and symptoms, evaluation of clinical signs, and screening and testing. In Danny’s case, the priorities are medical evaluation for allergies and an ear, nose, and throat (ENT) specialist’s evaluation of his upper airway, posterior airway, and tongue-tie.
It is possible that allergies and airway obstruction could be the driving forces behind most of Danny’s signs and symptoms. It is important to address these medical concerns first, and use the process of elimination before we return to the dental considerations.
Conclusion
After we concluded our evaluation and determined the priorities, we discussed our findings and recommendations for medical evaluations to reestablish an open airway for Danny. The treatments will also help reestablish normal tongue posture, swallowing function, and cervical neck posturing. After that, we can assess temporomandibular and occlusal concerns to complete our clinical care.
By carefully evaluating both the associated medical as well as dental and joint concerns, we have thoroughly addressed all aspects of Danny’s signs and symptoms, ensuring the best possible course of treatment for him.