Peri-implantitis (probing depth and bone loss)Author bioStuart J. Froum, DDS, whose private practice is limited to periodontics and implant dentistry in New York City. Dr. Froum, a diplomate of the American Board of Periodontology, is currently a clinical professor in the Department of Periodontology and Implant Dentistry at the New York University Krieser Dental Center, as well as the director of clinical research in the Department of Periodontology and Implant Dentistry at the New York University Dental Center. He is the past president of the Northeast Society of Periodontics and is on both the Research Committee and the Continuing Education Oversight Committee of the Academy of Osseointegration. Dr. Froum is a trustee of the American Academy of Periodontology and the recipient of several awards: Hirschfeld Award from the Society of Periodontologists, the Clinical Research Award for 2004 and 2005, and the William J. Gies Award for 2006. You may contact Dr. Froum by email at [email protected].
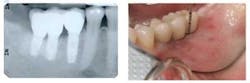
By Stuart J. Froum, DDSThis complaint is being heard more and more frequently by dentists and hygienists, either at routine recall maintenance visits or emergency visits. The most common cause of these complaints is that the implant and surrounding mucosa are suffering from mucositis or peri-implantitis. The two disease entities are accompanied by inflammation in the soft tissue around an implant(s) (mucositis) or soft-tissue inflammation combined with loss of bone around the implant (peri-implantitis). In some cases, these diseases can occur without discomfort or pain, similar to gingivitis and periodontitis. However, each of these diseases should be diagnosed and treated as early as possible to avoid more serious deterioration or even loss of the implant and restoration.Mucositis is manifested by redness, inflammation, and occasionally soreness in the soft tissue around the implant. It is caused by bacteria and is completely reversible. Effective oral hygiene and cleaning of the implant surface and sulcus can eliminate mucositis and return the peri-implant mucosa to a state of health. Two studies revealed mucositis occurs in more than 50% of implants placed.Peri-implantitis is the more severe entity and has been shown to occur in 11% to 47% of implants after five years in function. The diagnosis of this disease includes probing depths (PD) of 5 mm to 6 mm or greater, bleeding on probing, and bone loss greater than or equal to 2 mm to 3 mm around the implant. Mobility is not a good indicator of peri-implantitis, since an implant can lose 75% or more of its bone and still be immobile. Treatment depends on the extent of PD and bone loss. This is why at each recall visit, a dentist or hygienist should probe around the implant as they would probe around a natural tooth and record the pocket depth, bleeding, and presence of exudate. Radiographs should be taken of any implant exhibiting one or more of these symptoms and bone loss evaluated.Risk factors for peri-implantitis include poor oral hygiene, smoking, a history of periodontitis (even if treated), genetic susceptibility, poorly fitting restorations, retained subgingival cement on a cement-retained implant restoration, and poorly controlled diabetes. Patients must be told of the risk of peri-implantitis in the informed consent and informed of the methods they can use to prevent this disease. However, if allowed to progress, treatment of peri-implantitis usually entails removal of the implant-supported restoration followed by rebuilding lost bone and soft tissue and, if possible, replacement of the implant. All of this is time-consuming, very costly, risks litigation, and creates an unhappy patient.Methods to save a peri-implantitis-affected implant have been unpredictable at best. Recently, a technique to decontaminate a peri-implantitis-affected implant surface — combined with use of bone grafts, tissue modulators, and membranes or soft-tissue grafts — has shown promising results. These have been documented by the author of this article, Dr. Scott Froum, and Dr. Paul Rosen, and have been submitted for publication. This paper, combined with the information in the book “Dental Implant Complications: Etiology, Prevention, and Treatment” published by Wiley Blackwell and edited by this author, presents an in-depth review of the early diagnosis and treatment of mucositis and peri-implantitis.In addition, a one-day symposium on Dental Implant Complications will be held on Friday, March 23, 2012, in New York City to present the newest techniques to diagnose and treat peri-implantitis as well as other common dental implant complications including esthetic, prosthetic, surgical, treatment planning, and hard- and soft-tissue complications. Any dentist who places and/or restores implants today should consider attending this course as these complications will be seen more frequently due to the increase in the number of implants being placed and restored, combined with more aggressive protocols — i.e., immediate implant placement, immediate provisionalization, and immediate loading.The knowledge and experience of what to do when mucositis and/or peri-implantitis is diagnosed can make a significant difference in patient satisfaction, referrals, and overall profit to dentists wishing to build or expand their implant practice.