Dental labs can keep you informed about vast changes in technology. Rely on them when you consider treatment options for patients.
By Sharon Morgan, DDS
A successful partnership between a dentist and technician is crucial to the successful delivery of prostho-dontic treatment. The role of a technician has expanded in recent years to include the provision of information in the rapidly developing area of digital technologies. As practicing dentists, we know it is difficult to stay abreast of the changes in dental technology. We must rely on professional laboratories to counsel us as we consider treatment options for our patients.
The following case discussion is an example of recently available technologies that significantly enhance the quality of care we provide.
A 66-year-old man presented as a new patient for implant restoration evaluation. His medical history was significant for arthritis, emphysema, and depression. He had been edentulous in the maxillary arch for about six years after a long struggle with periodontal disease, and he had been wearing a maxillary denture with little success since that time. After going without any dental care for six years, he self-referred back to his previous periodontist, who then placed several Nobel-Biocare implants in his maxillary arch.
Teeth remaining in the lower arch were Nos. 20, 21, 22, 27, 28, and 29. He had a failing PFM splint from No. 22 to No. 27. Tooth No. 22 was deemed nonrestorable, and No. 28 was borderline restorable.
During the consultation appointment, we discussed several treatment options for the maxillary arch, including an implant-supported, full-arch splint, a full overdenture on implant-supported locator attachments, and an overdenture on an implant-supported bar with locators. The patient declined the fixed-splint option but thought the bar-overdenture was attractive in regard to stability and cost.
The patient was opposed to wearing a mandibular removable appliance and wanted to minimize further implants in the lower arch. We decided to try to retain teeth Nos. 20, 21, 27, 28, and 29 and to place two implants in the anterior mandible to restore the lower arch to premolar occlusion. The patient was then referred back to his periodontist for crown-lengthening procedures on teeth Nos. 20, 21, 27, 28 and 29 and for removal of tooth No. 22. He was also referred to an endodontist for root canal treatment on No. 28. An alginate impression was made for fabrication of a temporary acrylic mandibular partial .
The patient returned in a month for caries removal on teeth Nos. 20, 21, 27, 28, and 29. All five teeth were temporized with acrylic temporaries, and the temporary acrylic partial was delivered. The patient was then referred again to his periodontist for placement of two Nobel Biocare implants in the anterior mandible.
A preliminary alginate impression of both arches was taken during the following appointment. The arches were not restored concurrently because the patient was unable to wear his old maxillary denture in immediate need of a new maxillary denture. A custom tray was fabricated for the upper arch.
Five implant-level impression posts were placed, and a final open tray impression was made using 3M™ ESPE™ Imprint™ II impression material. Analogs were attached to the impression posts and the impression was sent to the lab for fabrication of a master cast. The lab returned upper and lower wax rims to be used in recording a bite registration.
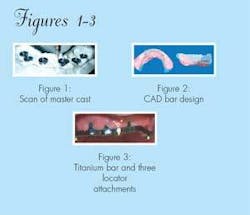
The patient returned for the bite registration, shade, and mold selection, and anatomical markings (midline, high lipline) using the wax rims. The lab was requested to fabricate a custom-milled, titanium bar to connect the five implants to include at least three Zest Locator Attachments arranged on the bar in a triangulated arrangement to provide retention and stability. The lab was also directed to prepare the maxillary denture set up for try-in using Dentsply Bioform anterior and anatoline posterior teeth. A model of the previous unserviceable denture was provided to serve as an esthetic guide as well as a matrix for the external dimensions of the CAD aspect of the 3i CAD/CAM titanium bar.
Bar fabrication
The CAD/CAM process developed by 3i (Implant Innovations, Inc.) has revolutionized the treatment of fully edentulous patients. The master cast and approved wax set up (in this case, a study model) is sent to 3i by the laboratory for scanning. Upon completion of the scan, the design is sent to the lab for evaluation and approval. Upon approval, the bar is machined from a solid block of titanium (see Figs. 1-3). The benefits of this technology include improved precision of adaptation, passive fit, density, and biocompatibility. The cost factors are similar to conventional laboratory castings when considering the cost associated with components, precious alloy, and technician labor.
When the patient returned for the try-in appointment, healing caps were removed and the custom-milled, titanium bar was seated. The precision fit was verified radiographically, and the denture wax-up was tried in and checked for esthetics and correct occlusion with the existing mandibular provisional restorations.
Lab processing
The SR-Ivocap resin processing system continues to represent the state-of-the-art in acrylic processing for prosthetic appliances. The injection method allows continuous feed of fresh acrylic during the curing stage. This eliminates the typical distortion associated with curing shrinkage. It is especially important when curing RPD or overdenture attachments to assure inter-attachment accuracy and successful prosthesis delivery (see Figs. 4-7).
Clinical delivery
At delivery, the healing caps were removed and implant sites were irrigated and inspected for debris before placing the titanium bar. The bar was placed and secured with gold-tite screws, tightened to 35 Ncm. The denture was then snapped to place on the three locators on the bar as the male attachments had been processed into the denture by the lab. Minor occlusal adjustments were done as the patient only had five remaining provisionalized mandibular teeth.
In the meantime, his periodontist had placed two Nobel Biocare implants in the anterior mandible at sites Nos. 23 and 25. While waiting for osseointegration, the patient returned for restoration of teeth Nos. 20, 21, 27, 28, and 29. A pre-op occlusal record was made using the previous mandibular wax rim. An impression was made using 3M ESPE Imprint II and the lab-fabricated splinted PFM crowns for teeth Nos. 20, 21, 27, 28, and 29. The splinted crowns were cemented with a very light coat of TempBond NE cement. The patient continued to wear his temporary acrylic partial.
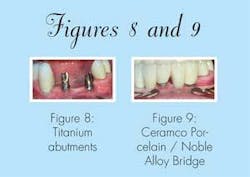
After five months of healing, an implant level, open-tray impression was made using 3M ESPE Imprint II material. The lab was instructed to fabricate custom CAD/CAM titanium abutments on implants at Nos. 23 and 25 and a PFM cantilever splint to restore Nos. 22, 23, 24, 25, and 26. Because of space limitations and the placement of the implants, the splint was fabricated as four units for the five-tooth space.
Lab procedure
A soft-tissue cast was fabricated and sent to 3i for fabrication of CAD/CAM titanium custom abutments for sites Nos. 23 and 25. The benefits of this process compared to conventional laboratory fabrication are the same as the overdenture bar previously discussed. The benefits of this technology include improved precision of adaptation, passive fit, density, and biocompatibility. The cost factors are similar to conventional laboratory castings when considering the cost associated with components, precious alloy, and technician labor (see Figs. 7-9).
Upon receiving the completed abutments, Drake Laboratory fabricated a four-unit Ceramco porcelain-fused-to-noble alloy splint, restoring teeth Nos. 22-26.
Clinical delivery AB
The patient returned for placement of the implant abutments and mandibular anterior splint. Healing caps were removed from Nos. 23 and 25, and the sites were irrigated and checked for debris. Then the abutments were placed on the implants and screws were tightened to 35 Ncm.
The PFM splint was placed on the implants with an impressive passive fit. Minor adjustments were made to the occlusion, and the splint was seated with a light coat of TempBond. With no further adjustments needed, the splinted crowns on teeth Nos. 20, 21, 27, 28, and 29 were cemented with Ketac cement.
This successful result illustrates the benefits of CAD/CAM technology in fixed, partially edentulous and fully edentulous implant therapy - two of several indications for custom-milled abutments for multiple implants. The accuracy that open-tray impressions produce combined with the precision fit of custom-milled titanium abutments and overdenture bar connectors result in a prosthesis with a passive fit and ultimate titanium biocompatability at all the connections.