Porcelain vs. Polyceramics
Polyceramic composites have been around for over half a century. They were first used for small fillings as early as the 1950s. While early materials filled the need for tooth-colored material, they lacked in the areas of strength, stability, and wearability. Composite technology has come a long way in 50 years. Today, we use composites (direct and indirect) with ease and predictability. If composites are ideal for standard dentistry, why wouldn't we want to consider them for implant restorations? In fact, polyceramics are an exciting choice for implant restorations. They work better than porcelain by producing a more predictable, profitable result for the technician, the dentist, and the patient.
The primary and most common material used for implant restorations is porcelain. Porcelain is a beautiful material that has been used successfully for decades. It seems unlikely that we would want to replace this material, but upon closer examination, factors exist that might cause us to reconsider using porcelain at least for implant restorations.
The main factor for choosing a polyceramic material over porcelain would be its lack of both brittleness and hardness. In terms of comparison to tooth structure, porcelain is three times more brittle. In surface hardness tests on the Vickers scale, porcelain comes in at 475 while tooth enamel is at 110. In an implant situation, the periodontal ligament is not available to cushion any of the trauma of mastication. A more resilient material will put less stress on the integrated implant and surrounding bone.
Another major factor in choosing a polyceramic material over porcelain is the wear on the opposing dentition. Porcelain is extremely abrasive. The new generation of polyceramic materials will wear significantly less than their porcelain counterparts. Can we replace porcelain as the restorative material of choice and still achieve pleasing esthetics?
Alternative to porcelain
Composites have always been esthetically pleasing, but they suffer from an image crisis. To appreciate the polyceramics of today, we must challenge our ways of thinking. The old paradigm held that composites had problems with strength, color stability, and shrinkage. That was true, but with today's technological advances, these materials are routinely prescribed for all types of ceramic restorations; i.e., inlays, onlays, bridgework, and crowns. The new paradigm states composites are strong, color-stable, and hydrophobic.
The real difference in today's formulations is the resin. Early generations used resins that were amorphous and brittle. They were made for smaller, tooth-colored fillings. They were never intended to be used for traditional crown and bridge buildups, or applied to implants. Composites are now available that have an internal matrix due to the use of microcrystalline resins. When these resins are combined with ceramic fillers, the result is an exciting balance of beauty and strength.
An excellent choice for implant restorations is DiamondCrown™, manufactured by DRM Research Laboratories, Inc., in Branford, Conn. DiamondCrown™ has many properties that make using this polyceramic material ideal for implant restorations. The resin in this polyceramic has a microcrystalline structure that adds three times the fracture resistance of porcelain fused to metal. This crystalline structure also creates a tough, resilient internal matrix.
The DiamondCrown™ material is also super-hydrophobic and 0 percent cytotoxic. These features eliminate fears about color stability and biocompatibility. Perhaps the greatest advantage in implant use is the wear factor. The hardness of this material is 110, exactly the same as natural tooth enamel. In an application such as an implant, where force dissipation is critical, it makes sense to look at a resin-based material.
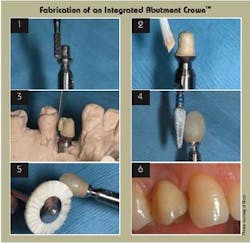
Fabrication of an Integrated Abutment Crown™
An Integrated Abutment Crown™ (IAC) is created by fusing successive layers of DiamondCrown™ onto a Bicon abutment. Bicon has pioneered the use of polyceramics as one of its restorative technique options, the IAC. The Bicon implant abutment connection uses a 1.5° locking taper. This locking taper offers 360° of universal abutment positioning. The technician can modify the abutment as necessary and build a crown without worrying about screws, screw chimneys, or timing issues. This permits the technician to prepare the margin at whatever level is needed to achieve superior esthetics.
The procedure begins by preparing a Bicon nonshouldered abutment. A carbide bur is used to reduce the bulk and define the margin (Figure 1).
Following preparation, the abutment is opaqued to mask out metal shadowing. The opaque procedure includes a metal coupler step that ensures a proper bond (Figure 2). Following opaquing, building is similar to porcelain ceramics. The crown is fabricated using opaque dentin, dentin, and enamel. The handling of composites is different from conventional ceramics — the technician must work the material with a spatula to mold and blend (Figure 3).
The shade is achieved by the addition of the different layers of dentin and enamel. Next, the material is cured in the light-cure booth. Following the buildup, the shape is refined by the use of carbide burs. The material carves very easily, and since there is very little shrinkage, the technician can build the crown to form (Figure 4). After refining the shape, the crown is polished with wheels and brushes (Figure 5). The final result is esthetically pleasing and functionally superior (Figure 6).
Laboratory procedures for fabrication of the IAC are not complex. In fact, since there are no metal frameworks to wax, less time is required than with conventional techniques. The labor savings can translate into less cost for the dentist.
An IAC restoration provides a distinct time-saving advantage. Seating the IAC takes significantly less time due to the screwless and cementless restoration. If an addition is needed for insufficient contacts, it is an easy chairside procedure.
Technological advances have made it possible for polyceramic implant restorations to esthetically replace teeth while preserving the surrounding dentition and supporting bone. This technique offers real benefits to everyone on the implant team, especially the patient.
George Zoller, CDT
Mr. Zoller owns a high-quality composite restorative laboratory in Asheville, N.C. He teaches polyceramic techniques to lab technicians worldwide. You may contact him by phone at (828) 670-8222 or by email at [email protected].