How trauma led to a classic case of external resorption: An endodontics case report
Dr. Stacey Simmons describes an endodontics case of a patient who presented to her office having sustained trauma to the facial and maxillary anterior area. She demonstrates how the history of a tooth helps obtain a definitive diagnosis of external resorption.
Editor's note: This article first appeared in DE's Breakthrough Clinical with Stacey Simmons, DDS. Find out more about it and subscribe here.
A healthy 40-year-old male presented to the office on an emergency basis. He had sustained trauma to the facial and maxillary anterior area.
Clinical and radiographic assessment revealed the following (figure 1):
- Complete loss of tooth No. 10 (the patient did not know where the tooth went upon impact).
- Significant swelling in the maxillary and mandibular labial areas with bruising and slight lacerations on the lip and tongue, which were caused when the lower teeth impacted the maxillary teeth with the tongue in between.
- A significant lingual laceration of papilla interproximal to Nos. 8 and 9 with possible involvement of the incisive nerve. Bone exposure was evident.
- Partially avulsed and lingually displaced tooth No. 9 with Class 4 mobility. There was tissue retention only (very light and unstable).
- All other teeth mesial and distal to No. 9 appeared secure.
- Radiographic assessment revealed a horizontal fracture of the alveolar interproximal bone between Nos. 9 and 10 at the apical one-third area. Tooth No. 9 was separated from the alveolar bone with partial avulsion. It was unclear whether the root tip was fractured.
- The patient was unable to bite down due to the mobility and lingual position of No. 9.
Figure 1
The key in this situation—and any emergency trauma, for that matter—is to first stabilize the patient and the affected area. Local anesthesia was delivered, the raw edges of the lacerated tissue were removed, and sutures were placed to bring the tissue together. A light orthodontic wire was bonded from Nos. 6 through 11, and one between Nos. 8 and 9 for more stability (figures 2 and 3). Appropriate meds were dispensed with follow-up instructions. The patient and his wife were informed that the prognosis for the tooth was questionable—primarily because of its displacement in the alveolus, which was also fractured. An assessment in 12 to 14 days was recommended.
Twelve days later, the patient returned with the following assessment and treatment (figure 4):
- Overall, the patient was feeling better, with reduced swelling in all soft-tissue areas.
- Chief concern: His bite was off. This was adjusted.
- Cold testing: No response with No. 9 and slight delay with No. 8.
- Tooth appeared more stable within the alveolus; the splint was removed between Nos. 8 and 9, but not from canine to canine.
- It was recommended that we commence with endodontic treatment on No. 9 and maintain a watch on No. 8 for any irreversible changes.
- Tooth No. 9 was opened up; the pulp was necrotic. The chamber was cleaned out, irrigated, and calcium hydroxide medicament was placed. It was recommended that we change out the dressing two to three more times over the course of the next few months, so stabilization of the tooth could continue and a better prognosis could be determined.
Figure 4
The six-week post-trauma follow-up (figure 5):
- Teeth Nos. 6 through 8 all tested vital.
- No. 9 appeared to continue stabilizing within the bone.
- We changed out the calcium hydroxide dressing.
- Another four to six weeks of healing was recommended, with subsequent completion of root canal and orthodontics wire removal.
Figure 5
Five-months post-trauma (figures 6 and 7):
- The patient reports no pain except for slight, intermittent tenderness in the maxillary vestibule around the apex of Nos. 8 and 9.
- A root canal was completed with removal of the orthodontics wire. The tooth was solid in the bone with no abnormal movement in any direction.
- We discussed that even though the current status quo appeared favorable, there was still a guarded long-term prognosis due to the severity of the trauma. However, overall, the outlook was trending in a positive direction.
- Treatment options for the replacement of No. 10 were discussed: bridge, implant, etc.
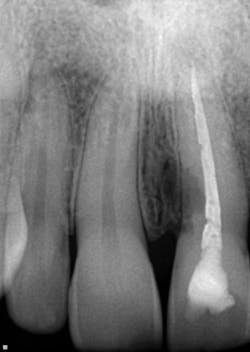
One-and-a-half years post-trauma (figure 8):
- The patient worked out of town for a period of time and then presented for his recare exam.
- The patient reported no concerns from his incident and was ready to move forward with tooth replacement.
- Radiographic examination of the maxillary anterior teeth revealed an uneven, corrugated-like radiolucency on the mesial aspect of No. 9 that extended just below the CEJ almost to the coronal half of the tooth.
- No. 9 was not tender to palpation, probing depths circa were 3 mm to 4 mm, and the bite test was normal.
Diagnosis: Trauma-induced external resorption
Figure 8
As discussed in a previous article that reviewed the differences between internal and external resorption, external resorption is “resorption initiated in the periodontium and initially affecting the external surfaces of the tooth—may be further classified as surface, inflammatory, or replacement, or by location as cervical, lateral, or apical; may or may not invade the dental pulpal space.” (1) Further, "it may arise as a sequel of traumatic injury, orthodontic tooth movement, or chronic infection of the pulp or periodontal structures.” (2)
In this case—based on the history behind this tooth, the fact that such a large portion of the tooth had so quickly resorbed, and knowing that the prognosis for a tooth with external resorption is poor—it was recommended that tooth No. 9 be removed. Replacement options were again discussed.
The patient opted to have a bridge from Nos. 8 through 11. Tooth No. 9 was extracted atraumatically, and assessment revealed a vast area of very destructive external resorption that had almost broken through to the pulp chamber. Although difficult to see, small horizontal fracture lines were noted on the distal side of the tooth, which supports the suspicion that the tooth sustained microfractures upon impact that subsequently led to the initiation of external resorption. Lastly, there was a large abscess at the apex of the tooth which, at first, wasn’t readily apparent on the radiograph (figures 9 through 12).
This case—although cut-and-dried—is an example that the history of a tooth (or area) does indeed aid in obtaining a definitive diagnosis of external, and internal, resorption. Treatment modalities, although limited, need to be comprehensively discussed so proper care can be administered.
References
1. Maria R, Mantri V, Koolwal S. Internal resorption: A review and case report. Endodontology. 2010;22(1):100-108. medind.nic.in/eaa/t10/i1/eaat10i1p98.pdf.
2. Kuo T-C, Cheng Y-A, Lin C-P. Clinical management of severe external root resorption. Chin Dent J. 2005;24(1):59-64.
Editor's note: This article first appeared in DE's Breakthrough Clinical with Stacey Simmons, DDS. Find out more about it and subscribe here.