Endodontic treatment of an upper first molar: materials, methods, and clinical challenges
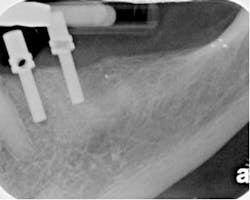
- The canals were moderately calcified.
- The apical half of the mesial buccal root was severely curved.
- The metal foundation of the crown obscured the pulp chamber.
- The crown’s porcelain was at risk of fracture during access procedures.
- The apex of the palatal root appeared to have periapical pathology that was inconsistent with the finding of extreme cold sensitivity. The palatal root appeared straight and relatively uncomplicated.
- Given that this is an upper first molar, it was expected to find an MB2 canal in the mesial buccal root.
The above findings provided the following challenges:
- The calcification present in all roots required significant time with hand K files to negotiate before rotary nickel titanium (RNT) files should be inserted.
- The mesial buccal root apex was especially susceptible for (RNT) file fracture due to its curvature and calcification.
- With the pulp chamber obscured, the risk of furcal perforation was high if the access was taken too far apically.
- Access through the crown required copious water and ultrafine diamonds to prevent fracture of the porcelain.
- The palatal root, if not carefully explored with regard to its length, could easily lead to overinstrumentation with a RNT file if inserted too rapidly without regard for the position of the minor constriction of the apical foramen (MC).
Additional clinical considerations
Additional preoperative clinical considerations to be addressed before access included the expected master apical taper and master apical diameter. The prepared master apical taper is a function of the anatomy as well as the RNT system being utilized. For RNT files that are manufactured by a grinding process and especially those with radial lands, the master apical taper is likely to be .06 along the length of the canal. For RNT files manufactured by a twisting process such as the Twisted File (SybronEndo, Orange, Calif.), it is both efficient and predictable to prepare a .08 taper in the mesial buccal (MB) and distal buccal (DB) canal and .10 taper in the palatal canal. Given that this tooth is vital yet irreversibly inflamed, the master apical diameter anticipated was approximately a #40 ISO tip size. How this master apical diameter was prepared is detailed below.
Clinical management
- Before starting, an estimate of the true working length was determined from the initial radiographs.
- After profound anesthesia, under the rubber dam and surgical operating microscope (SOM) (Global Surgical, St. Louis, Mo.), access was made with copious water spray. An alternative to the SOM would have been the use of HiRes 4.8X Class IV Orascoptic loupes with a light source (Orascoptic, Middleton, Wisc.). In any event, whether provided by loupes or the SOM, the value of lighting and magnification in access and subsequent treatment cannot be overstated.
- The porcelain of the crown did not fracture using ultrafine diamonds. Once the pulp chamber was reached through the crown, a diligent effort was made to expose the various canal orifices and to provide straight-line access. The cervical dentinal triangles of the mesial buccal, distal buccal, and palatal canal were removed using TF (.10/25 for the palatal and .08/25 TF for the buccal roots) in a brushing motion up and away from the furcation.
- TF was used to shape the coronal third of the three roots. After coronal third shaping, the MB, DB, and palatal roots were explored with a #8 hand K file and apical patency was assured. Once the #8 hand K file reached the estimated working length, an electronic apex locator determined the position of the true working length (TWL). A glide path for TF was prepared using the M4 Safety® Handpiece (SybronEndo, Orange, Calif.) to reciprocate hand K files to the diameter of a #15 hand K file.
- The roots were instrumented crown down with the .08/25 TF to prepare a .08 master apical taper followed by a #40 master apical diameter. The sequence in all canals was virtually identical; a .08/25 was inserted to the TWL in approximately four insertions followed by a .06/30/35 TF and .04/40 TF, each inserted once. The smaller taper of the .04 and .06 TF fit easily and predictably to TWL in each canal. The .06/30/35 TF and .04/40 TF files cut only on their tips at the apex. Working length was confirmed with electronic measurements once the first TF (.08/25) and last TF reached the TWL.
- The MB orifice was immediately visible upon access slightly off to the mesial of a straight line between the MB orifice and the palatal orifice. The first file into the MB2 canal was the #6 hand K file inserted with gentle pressure. This #6, as were all hand K files, was precurved with an Endo-Bender® (SybronEndo, Orange, Calif.). The #6 initially made slight progress down the MB2. The file was withdrawn, the orifice irrigated, and another precurved #6 inserted. A repetition of this action allowed a #6 hand K file to reach the apex with several insertions. Next, a #8 hand K file was inserted into the MB2 and reciprocated, followed by a #10 hand K file until both spun freely. An electronic determination of TWL was obtained in the MB2 once the #10 hand K file reached the estimated working length. The MB1 and MB2 merged at mid-root. The MB2 was enlarged to a .08 taper with a .08/25 TF and its master apical diameter confirmed to a #40.