Managing black tartar and tooth stains: A challenge for dental professionals
As dental professionals, managing black tartar and other tooth stains is an ongoing challenge. Although often seen by patients as a cosmetic issue, these problems can severely impact oral health, leading to periodontal disease, tooth decay, and even tooth loss if left untreated. Understanding the causes, prevention strategies, and effective treatments is essential in helping patients maintain optimal oral hygiene and overall health.
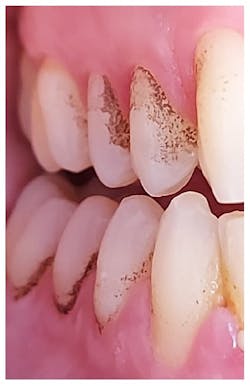
Tartar, or calculus, forms when plaque left on teeth hardens due to minerals in saliva. If not regularly removed, this hardened plaque can absorb staining substances, turning it dark. Smoking is a common cause of staining, but dietary factors such as coffee, tea, and red wine also contribute significantly.1,2
Black tartar typically forms below the gumline, where cleaning is more difficult. Once it develops, tartar provides a surface for bacteria to attach, which accelerates its accumulation. The challenge for dental professionals is to effectively remove this buildup before it leads to more serious oral health issues such as gum disease or infections.1,2
“Roughness on the tooth surface can easily stain, often due to smoking. Smokers also tend to hold tobacco in the same spot, leading to significant discoloration in specific areas of the mouth,” explains Emilia Kataja, MHS, RDH, oral health regional manager at Koite Health Ltd.
The role of antibacterial treatment
Studies show that several types of bacteria contribute to plaque buildup, which eventually hardens into tartar. Streptococcus mutans, for instance, produces acids that erode tooth enamel and promote tartar formation.2 Another significant bacterium, Porphyromonas gingivalis, is commonly associated with periodontal disease. It contributes to the formation of subgingival tartar, which often appears black due to mixing with blood from inflamed gums. Additionally, Actinomyces species are involved in the early stages of plaque formation and contribute to the hardening of plaque into tartar. Finally, chromogenic bacteria also play a role by producing pigments that stain tartar, giving it a dark appearance.2
“The unfortunate reality is that once these stains form, they can’t be removed by the patient on their own. Only a professional can effectively clean the rough areas and remove the stains. The easiest and most cost-effective way for patients to manage tartar and staining is through preventative oral hygiene,” emphasizes Emilia Kataja.
In addition to regular mechanical oral hygiene, antibacterial treatments are essential in managing plaque-related oral health issues. The Lumoral device* utilizes antibacterial photodynamic therapy (aPDT) combined with a photothermal effect to target harmful bacteria in the mouth. This helps reduce plaque formation and prevents the development of black tartar. By using the device regularly, patients can effectively manage bacterial loads in hard-to-reach areas, which can reduce the need for more invasive treatments later on.3
Enhancing oral care routines
As an oral health professional, incorporating Lumoral antibacterial treatment into a patient’s oral care routine offers a noninvasive, drug-free method to support and enhance their hygiene practices. Designed for at-home use, Lumoral complements regular brushing, interdental cleaning, and professional checkups to help maintain long-term oral health and reduce tartar buildup.
The antibacterial action of Lumoral is particularly effective in hard-to-reach areas and on implant surfaces, helping to reduce biofilm formation and tartar growth. Clinical studies have demonstrated its efficacy, with notable improvements in key indicators such as reduced bleeding on probing (BOP).3,4
According to Europe’s largest periodontitis study, more than half of the participants who used Lumoral were healed from gum inflammation based on the BOP index—2.5 times more than the control group who did not use the device. In the control group, only 22% of participants achieved healthy gums after three months. Lumoral users also experienced significantly less plaque buildup, while the control group showed no reduction in plaque levels.3
Additionally, two-thirds (67%) of Lumoral users reduced the number of deep gum pockets by half compared to their initial condition, achieving significantly better results than the control group. These findings underscore Lumoral’s value as a highly effective adjunct to traditional oral care methods.3
* Lumoral, which is not yet sold in the United States, is a CE-certified medical device, which means it meets the safety and health requirements set by the European Union. It is based on scientific research and is widely used both at home and recommended by professionals, ensuring its safety and effectiveness.
Editor’s note: This article first appeared in Clinical Insights newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe.
References
- Veses V, González-Torres P, Carbonetto B, et al. Dental black plaque: metagenomic characterization and comparative analysis with white plaque. Sci Rep. 2020;10(1):15962. doi:10.1038/s41598-020-72460-2
- Larson J. Why am I getting a black buildup on my teeth? Healthline. January 25, 2022. https://www.healthline.com/health/dental-and-oral-health/black-tartar-on-teeth
- Pakarinen S, Saarela RKT, Välimaa H, et al. Home-applied dual-light photodynamic therapy in the treatment of stable chronic periodontitis (HOPE-CP)–three-month interim results. Dent J (Basel). 2022;10(11):206. doi:10.3390/dj10110206
- Panzironi G. La terapia fotodinámica domiciliaria como medio de prevención para el control del biofilm. Zenodo. 2022.
About the Author

Nina Garlo-Melkas, MSc
Nina Garlo-Melkas, MSc, is a health and science journalist.