By Fred C. Quarnstrom, DDS, FADSA, FAGD, FICD, FACD, CDC, FACD
Local anesthesia is remarkably successful. However, we have all had patients who simply will not go numb. Somehow these patients always seem to be the ones who also are apprehensive. We all have pain inhibition systems and body-produced chemicals that help lessen pain, endorphins and serotonin being two groups of endogenous chemicals. There is some thought that part of the reason why these patients are apprehensive is because they always have trouble with anesthesia. Trauma always gives them more pain than other patients having the same procedure. There is some evidence that this is genetic.
It is very frustrating for both the patient and the dentist when it is impossible to get profound local anesthesia. Our scheduling is such that we need a predictable way to achieve anesthesia with all patients; no one likes to cause pain for their patients.
When the typical block or infiltration fails, intraosseous injections are an alternative. This technique has been described over many years using a variety of techniques and equipment.
- Early techniques required a large needle to perforate the cortical bone. Injection was then done into the medullary bone with this large needle.
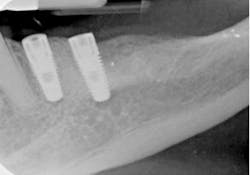
- Recently, devices became available that perforate the cortical bone with a needle that rotates in a slow-speedhand piece. A 31-gauge needle is then threaded into this hole and local anesthetic is injected into the medullary space (Figs. 1, 2).
- Another device injected local anesthetic through the needle that was used to perforate while it was attached to a handpiece.
- Some of us used PDL, periodontal ligament, injections when anesthesia failed. A needle was threaded into the bone adjacent to the tooth root and local anesthetic was injected. Some felt it was important for the bevel of the needle to be toward or away from the root. I had assumed that the local stayed in the PDL space and worked its way to the apex of the root where it blocked the nerve entering the root. A later study showed that it was an intraosseous injection. When the solution was tracked, it had entered the medullary space and did not stay in the PDL space. The PDL space we see so clearly in X-rays is an X-ray artifact. The tooth socket does not have a dense lining of bone.
- First put a drop of local anesthetic in the attached gingiva distal to the tooth you want to anesthetize.
- Immediately perforate with the rotating perforator (Fig 3).
- Remove the perforator and thread a 31-gauge needle into this hole (Fig 4).
- Inject very slowly about 1 cc of local anesthetic. It is important to inject very slowly as the drug is absorbed almost as rapidly as if it were injected intravenously (Fig 5).
- The tooth is numb within seconds (Fig. 6, 7).