Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia (review)
Patients can colonize pathogenic bacteria within forty-eighty hours of admission to intensive care unit.(1) The oral cavity and other parts of the mouth are perfect medium in which bacteria can live and thrive.(1) Aspiration of orapharyngeal secretions is an independent risk factor for ventilator associated pneumonia (VAP) and is documented as being a major cause of nosocomial infection in the ICU.(2) It has been shown that bacteria responsible for VAP collect and colonize on the oral mucosa and in the dental plaque biofilm of intubated patients.(3) Providing adequate oral care for these patients should be a priority as it is essential in reducing incidences of VAP.
Philips Respironics V200 critical care ventilator and Respironics NM3 respiratory profile monitor
According to the authors of a recent Cochrane Review, ventilator-associated pneumonia (VAP) is defined as pneumonia developing in persons who have received mechanical ventilation for at least 48 hours.(4) VAP is a potentially serious complication in these patients who are already critically ill.
Maintaining a clean and healthy mouth by preventing the build-up of plaque biofilm on the teeth may help reduce the risk of developing VAP. Oral hygiene care (OHC), using either a mouthrinse, gel, toothbrush, or combination, together with aspiration of secretions may reduce the risk of VAP in these patients.(4) The objective of the review was to assess the effects of OHC on the incidence of VAP in critically ill patients receiving mechanical ventilation in intensive care units (ICUs) in hospitals.
The question was whether oral hygiene care could reduce the incidence of ventilator-associated pneumonia (VAP) in critically ill patients receiving mechanical ventilation in intensive care units (ICUs) in hospitals (excluding the use of antibiotics). The intent was to summarize the available suitable research in order to facilitate the provision of evidence-based care for these vulnerable patients. Trials were grouped into four main comparisons:
1. Chlorhexidine antiseptic mouthrinse or gel compared to placebo (treatment without the active ingredient chlorhexidine) or usual
care, (with or without toothbrushing).
2. Toothbrushing compared with no toothbrushing, (with or without chlorhexidine).
3. Powered compared with manual toothbrushing.
4. Oral care with other solutions.
Hence, there is a clear need for more research to develop guidelines to influence practice and more education is required to stress the importance of oral care in intubated patients.(5) Guidelines should be evaluated for their effect, value and usage, and reviewed and modified regularly to incorporate new evidence that becomes available.
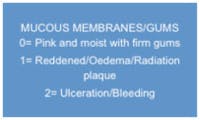
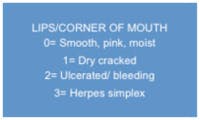
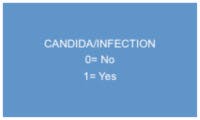
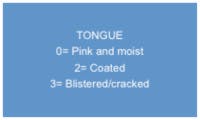
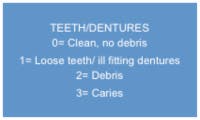
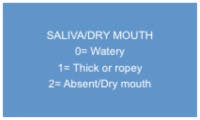
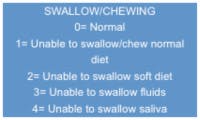
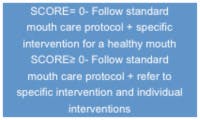
Daily oral care health assessment adapted.(6)
References 1. Prendergast,V., Hallberg, I.R., Hagell, P., Jahnke, H., Kleiman, C., 2009.Oral health, Ventilator associated pneumonia and intracranial pressure in intubated patients in neuroscience intensive care unit. American Journal Of Critical Care, 18(4), pp 369 – 376. 2. Berry, A. M., Davidson, P.M., Masters, J., Rolls, K., 2007. Systematic literature review of oral hygiene practices for intensive care patients receiving mechanical ventilation. American Journal of Critical Care, 16(6), pp 552 – 562. 3. Kishimoto, H., and Urade, M., 2010. Assess Dental plaque and suction- Etricated bacteria adequately. Chest, 137(1) pp 500. 4. Shi Z, Xie H, Wang P, Zhang Q, Wu Y, Chen E, Ng L, Worthington HV, Needleman I, Furness S. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database of Systematic Reviews 2013, Issue 8. Art. No.: CD008367. 5. Njoroge N and Paul F. Reducing Ventilator Associated Pneumonia (VAP): The Importance Of Oral Care In Mechanically Ventilated Patients. ICU Management, Volume 11, Issue 1, Spring 2011. 6. Pear, S.M., Stoessel, K., Shoemake, S., 2007. Oral care is critical care: The role of oral care in the prevention of hospital acquired pneumonia. Infection Control Today, 11(10).