A community-based response to municipal water defluoridation
By Roopsi Narayan, MPH ǂ, Donald E. Brannen, PhD, †‡, Dean Olson, MD, MS, MS¶, Janice Gray ‡, *, Robyn Fosnaugh ‡, and Melissa Howell, MPH, MBA, MS, RN, RS
ǂ Center for Global Health, Department of Community Health, Wright State University Boonshoft School of Medicine; ‡ Greene County Combined Health District, Greene County, Ohio; ¶ Division of Aerospace Medicine, Boonshoft School of Medicine, Wright State University; * Yellow Springs Retired Physician; • Yellow Springs Schools, ∆ Yellow Springs Village Council, † Greene County Medical Reserve Corps, Greene County, Ohio.
Abstract
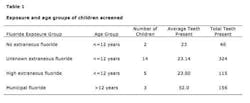
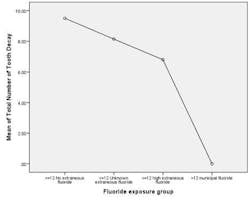
In February 2011, the Village of Yellow Springs stopped municipal water fluoridation. By December 2012, community stakeholders came together to conduct dental surveillance for children in the third and eighth grades. Children without access to municipal fluoridation had greater amounts of tooth decay among permanent and primary teeth (n=24, p=.004). Children had 2.98 less cavities for every increase in fluoride exposure category (correlation coefficient = 0.83). Challenges of this longitudinal, community-based program include obtaining time to conduct screenings within the school’s busy teaching schedule, compliance of parents/guardians completing the exposure survey, collaborator attrition, and obtaining adequate resources. The next steps for the community are continued dialogue to address the impact of local water fluoridation on children’s health.
Key Words: Dental Caries, Longitudinal Studies, Public Health Surveillance
Introduction
Fluoride is a natural element found in rocks, soil, freshwater, ocean water, and is important to the integrity of bone and teeth. The Centers for Disease Control and Prevention (CDC) has recognized water fluoridation to be one of the 10 great public health achievements of the 20th century and that optimal fluoridation has been a major factor in the decline of tooth decay (Centers for Disease Control and Prevention, 2006). While some communities have naturally occurring optimal fluoride levels, most do not. The primary role of fluoride is the prevention of dental caries. Tooth decay results when bacteria colonized on tooth surfaces metabolize sugars and refined carbohydrates to acids, resulting in removal of minerals from the surface of the tooth (Palmer & Gilbert, 2012). Fluoridation of public water supplies continues to be safe, effective, and the least expensive way to deliver the benefits of fluoride to a community (Griffin, Jones, & Tomar, 2001). Fluoridation is cost-effective because it saves money on dental treatment needs; ensures that all people, regardless of age, income, education, or race, receive fluoride benefits; and guarantees that everyone in the community benefits, especially those who do not receive regular dental care. Studies have shown that fluoridation reduces tooth decay by about 25% over a person’s lifetime (Brunelle & Carolos, 1990).
RELATED | ADA revises fluoride suggestions for young children
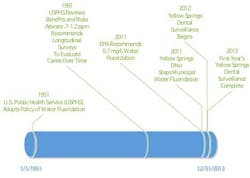
In 1991, the United States Public Health Service recommended water fluoridation of 0.7 to 1.2 parts per million and the initiation of longitudinal studies if a community decides to not add fluoride to their water supply (USPHS, 1991). In response to stopping fluoridation of municipal water supply of a local village, a prospective cohort study was developed to track exposures to fluoride and survey children through their primary tooth development phase.
Study area
The Village of Yellow Springs in Greene County, Ohio, holds routine community hearings. In response to a motion to stop municipal water fluoridation, the county public health agency presented results from a 16-year retrospective review. The report indicated an increase in bone related cancers (2.9 vs. 2.1 per 10,000 persons; p=.0493) and an overwhelming number of dental caries in persons from the nonfluoridated areas (Brannen & McDonnell, 2009). While this internal report was on unadjusted rates and is unpublished; it is readily reproducible as the data was on mortality of the areas by fluoridated status. The county public health agency recommended that a minimal level of fluoridation in the municipal water supply of 0.7 milligrams per liter be maintained. Heated discussions revolved around the lack of “hard evidence” linking fluoridation with improved dental health (Chiddister, 2010). The Village Council opted to discontinue fluoridating their water supply on February 22, 2011. This report includes efforts by Yellow Springs Village Council, School District, community residents, Wright State University, Cedarville University, the local Medical Reserve Corps unit, and the local public health agency to build a collaborative dental surveillance program and presents initial observations of some of the children’s dental health after water defluoridation occurred in Yellow Springs, Ohio.Fig. 1: An MRC volunteer and the GCCHD dental hygienist working. (Photo: Janice Gray and Julie Reynolds)
The project was approved on May 7, 2012, by the local public health agency, school authorities, and the Village Council. The first round of screenings of third and eighth grade students occurred on Dec. 17, 2012, and Jan. 8, 2013. Guardians were asked to sign consents prior to screening and to complete an exposure assessment. The dental team was comprised of Medical Reserve Corps volunteers and public health dental staff. Some costs to stakeholder agencies were offset through civic generosity, volunteerism, and student involvement.
ADDITIONAL READING |Tribal tribulation: An investigation into dental caries in third-world conditions
Fig. 2: Timeline of water fluoridation and dental surveillance (note mg/L can be expressed as ppm)
Fig. 3: Mean of child teeth with decay or indications of decay by exposure group through dental examination. Exposure groupings developed by exposure category through survey assessment.
Fig. 4: Mean of adult teeth with decay or indications of decay by exposure group through dental examination. Exposure groupings developed by exposure category through survey assessment.
Fig. 5: Total of adult teeth with decay or indications of decay by exposure group through dental examination. Exposure groupings developed by exposure category through survey assessment.
Limitations and use of findings
The response rate for each grade was less than 18%. Significant bias could be a factor between the 3rd and 8th grades, however, most of those observed were in the third grade. The number of exposure assessment was low, which required a surrogate metric of exposure to fluoride based upon matching the age commensurate with primary tooth development and time of municipal fluoridation. Another limitation is the low numbers of subjects in this first year of data does not allow for accounting of nesting of teeth in the analysis of total teeth affected. However, even with these limitations given the dramatic reductions in tooth decay, the authors felt it was an ethical imperative to present these early results. It is hoped that this report will allow for continued surveillance that will increase the number of subjects, thereby mitigating these limitations. Without further dental surveillance and exposure assessment, long-term surveillance of all cause morbidity will not be reasonable to expect. This is important because of the potential, although very rare except where inadvertent high exposures have occurred, for dental fluorosis. Dental fluorosis causes visible changes in the enamel surface of the tooth. One of the advantages of a cohort of children who are tracked over time is that other increases of disease can be explored to determine their association to fluoride. There is a pivotal need to address the concerns of those residents who have forebodings pertaining to water fluoridation.
The local public health agency in collaboration with the Village Council hopes that by providing the results from the first year’s data, residents can make informed decisions about local water fluoridation policies and practices. The strength of these findings given the low number of subjects (n=24), the consistency of results across statistical methods, and a strong dose response curve are indicative that children with exposure to municipal fluoride exposure had significantly less tooth decay.
Challenges and next steps
Multiple challenges are present when performing a study of this kind. Scheduling and conducting screenings are difficult when schools are busy meeting their primary responsibilities. The compliance of guardians completing the exposure assessment also presents challenges. Completion of the exposure assessments is time-consuming, but critical to measuring extraneous sources of fluoride. Some collaborative members have left and may continue to leave the project. Without long-time local practitioners, the project’s staying power over time is limited. The ability to fund this project called for creativity when addressing budget issues.
Once all the hard work of obtaining objective results is completed, delivery of the message remains the greatest challenge. Getting all sides of the ongoing fluoridation debate to use the surveillance results for making informed decisions will be difficult, as it may not be what some members want to hear. Ultimately, the surveillance may help build relationships within the community that result in improved health of the children.
Roopsi Narayan, MPH, is an MPH student, originally from India, and now a Greene County resident completing her graduate work. Dean Olson, MD, MS, MS, is director of the Division of Aerospace Medicine, Boonshoft School of Medicine, Wright State University, the oldest civilian aerospace medicine program in the United States. Janice Gray is a dental assistant at the Greene County Combined Health District. Robyn Fosnaugh is the director of Community Health Services at the Greene County Combined Health District. Melissa Howell, MPH, MBA, MS, RN, RS, is the health commissioner of Greene County Combined Health District, Greene County, Ohio. Donald E. Brannen, PhD, is the epidemiologist for Greene County Ohio and Unit Leader for the Greene County Medical Reserve Corps, Greene County, Ohio.
References
Brannen DE, McDonnell MA. Retrospective cohort study of Greene County residents and osteosarcoma. 2009. Unpublished manuscript, Greene County Combined Health District, Xenia, Ohio.
Brunelle JA, Carolos JP. Recent trends in dental caries in U.S. children and the effect of water fluoridation. Journal of Dental Research 1990; 69;723-727.
CDC. (2004). Surgeon general’s statement on community water fluoridation. Retrieved from http://www.cdc.gov/fluoridation/fact_sheets/sg04.htm
CDC. (2012). Fluoridation basics. Retrieved from http://www.cdc.gov/fluoridation/benefits/background.htm
Centers for Disease Control and Prevention (CDC). Fluoridation: Nature’s way to prevent tooth decay. 2006. Retrieved from http://www.cdc.gov/fluoridation/pdf/natures_way.pdf
Chiddister D. (January 27, 2011). Yellow Springs: Council says no to fluoride. Retrieved from http://www.fluoridealert.org/news/yellow-springs-council-says-no-to-fluoride/
Griffin SO, Jones K, Tomar SL. An economic evaluation of community water fluoridation. Journal of Public Health Dentistry 2001;61(2):78-86.
Palmer CA, Gilbert JA. Position of the academy of nutrition and dietetics: The impact of fluoride on health. Journal of the Academy of Nutrition and Dietetics 2012;112(9):1443-1453.
USPHS, 1991. Review of Fluoride: Benefits and Risks. Report of the ad hoc subcommittee on fluoride of the committee to coordinate environmental health and related programs. United States Public Health Services, Department of Health and Human Services, February 1991. Retrieved from http://www.health.gov/environment/ReviewofFluoride/default.htm
Websites
Fluoridation basics. Centers for Disease Control and Prevention Website. http://www.cdc.gov/fluoridation/basics/index.htm Published 2013. Updated July 25, 2013. Accessed July 26, 2013.
Surgeon general’s statement on community water fluoridation. Centers for Disease Control and Prevention website. http://www.cdc.gov/fluoridation/factsheets/sg04.htm Published 2004. Accessed May 4, 2013.