WRITTEN BY
Roxanne P. Benison, DMD, MS
Epidemiological data reveal that splits or fractures are the third most common cause of tooth loss in industrialized countries. This finding indicates that the cracked tooth syndrome is of high clinical importance.
Etiology
Cracked teeth can be one of the most difficult sources of dental pain to diagnose. When the pain is referred to, patients often find it difficult to pinpoint the source of pain to a specific quadrant, frustrating both the clinician and patient. In 1964, Cameron 1 coined the phrase “cracked tooth syndrome” (CTS), describing the pain as originating from a hairline or incomplete fracture of the tooth. A lack of awareness about the condition, coupled with its various clinical features, can make diagnosis of CTS difficult2 CTS usually causes pain when occlusal forces are placed upon portions of the tooth, causing dentin involved in the fracture to be exposed momentarily, resulting in a change in hydrostatic pressure within the dentinal tubules.
Figure 1
Cracks or fractures can be the result of a variety of habits. Grinding, clenching, and ice chewing over extended periods of time can cause extensive damage to the teeth, with cracks being a common result. Cracks can also be the result of an isolated incident such as biting into an olive pit or bone, or an accident resulting in trauma to the teeth. Although any tooth can be affected by a crack, the mandibular molars are the most prone to fracture. Heavily restored teeth or those with extensive decay are especially subject to cracks. One study evaluated the incidence of CTS in a general practice and found a far higher incidence of CTS in teeth that had the marginal ridge restored than those that had not.3 However, unrestored, noncarious teeth have also exhibited cracked tooth syndrome. Many morphologic, physical, and iatrogenic factors such as deep grooves, pronounced intraoral temperature fluctuation, poor cavity preparation design, and improper selection of restorative materials can predispose posterior teeth to an incomplete fracture (see Figure 1).4
Diagnosis
Whenever a patient has a complaint of intraoral pain and an obvious cause for that pain cannot be detected, it is prudent for clinicians to perform a comprehensive oral evaluation on these patients, since cracked teeth have frequently been associated with referred pain. Patients often report the pain as originating from a certain quadrant; however, vitality testing and radiographs are nonremarkable. Examination of the opposing quadrant may reveal the source. Performing a comprehensive examination can help eliminate misdiagnosis and/or mistreatment.
Historically, diagnosis of CTS has been primarily symptom based. 5 Visualization of cracks intraorally with the naked eye has proven difficult. Clinicians would encounter patients who complain of sharp shooting pains when they bite, or upon release of biting. Symptoms may also include sensitivity to cold food or drink. The problem with waiting for symptoms to develop before a diagnosis is made is that at this point the crack is usually at what is referred to by Clark5 as end-stage crack progression, requiring more aggressive treatment.
The emergence of the dental microscope has been a tremendous aid in the diagnosis and treatment of cracked teeth. The routine, methodical examination of the teeth with the microscope may help detect cracks in the early stages. When cracks are detected early they can be treated more conservatively and hopefully prevent the onset of symptoms. In addition to the microscope, many other tools are great aids in the diagnosis of cracked tooth syndrome, including (but not limited to) a bite stick, transillumination, and vitality testing.
A complete dental history is also sometimes informative. When patients are unable to identify the offending tooth or quadrant involved, the dental history can reveal numerous dental procedures with unsatisfactory results.2 This is sometimes a clue that the patient may be suffering from an undiagnosed cracked tooth. Furthermore, patients may recall an incident when they bit on a hard object that directly triggered the painful symptoms.
A fiber-optic wand or a handpiece equipped with a fiber-optic light can be useful in the detection of cracks. By holding the wand or handpiece horizontally at the gingival sulcus in a dimly lit room, the suspected crack may become more visible. Composite curing lights are generally too bright for this purpose and are not recommended.
If a tooth has a large restoration, it may be necessary to remove it to expose the crack. Methylene blue dye can sometimes be helpful. The dye should be applied to the occlusal surface of the tooth with a cotton roll or cottonwood stick. Have the patient bite down and move from side to side. The excess dye is then removed with alcohol. Further inspection may reveal the elusive fracture. The bite stick (Tooth Slooth or Crackfinder) is also an important tool in the diagnosis of cracks. The stick should be placed over each cusp and the patient should be instructed to bite down firmly; usually upon the release of pressure the patient will experience pain. Finally, vitality testing should be used to try and reproduce the patients’ symptoms and confirm your diagnosis.6
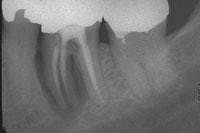
Figure 2
Radiographs usually are not helpful in the detection of cracks. They tend to be unremarkable in most cracks, because these fractures usually run mesiodistally and are not in the plane of the X-ray beam. Sometimes, however, the presence of a complete vertical root fracture can be seen radiographically (see Figure 2). These are cases where the crack extends beyond the crown of the tooth and down into the root. Here you may see a radiolucency involving the lateral aspect or halo surrounding the entire root. This can be differentiated from other radiolucencies by the fact that it surrounds the root uniformly, rather than being located at the portal of exit of the apical foramen or lateral canal. These cases are usually associated with a probing depth corresponding to the extent of the crack. This is the case when the crack is more extensive, long-standing, and the pulp is necrotic. Therefore, there will be no sensitivity to cold or sharp pain, only a dull ache on biting or pressure.7
Treatment
Figure 3
Treatment of the tooth depends on the degree of pulpal involvement and the extent of the crack. Those cracks, which are visualized but remain asymptomatic and clinical testing (such as percussion, palpation, mobility, probing, and thermal testing) is within normal limits, should be treated with a crown or some other form of complete cuspal coverage (see Figure 3). This is to prevent further propagation of the crack and the onset of symptoms. However, if a patient exhibits more extensive symptoms from the start, including increased sensitivity to thermal provocation and percussion/biting, root canal therapy should be performed prior to placement of a crown. These are considered incomplete vertical root fractures. A study by Kahler8 showed that all symptomatic cracks in teeth appeared to extend right through the dentin to the dentino-enamel junction and were extensively contaminated by bacteria. Hence, root canal therapy and crowning for all symptomatic cracks are recommended.
Upon initiation of root canal therapy, the tooth should be examined under a microscope to further evaluate the extent of the crack. Teeth that are considered restorable are those where the crack is confined to the crown portion of the tooth, coronal to the mucogingival complex. Cracks that extend across the furcation of the tooth, or those extending below the osseous crest, and/or are associated with a corresponding narrow deep pocket are complete vertical root fractures and have a poor prognosis. Teeth with complete vertical root fractures are considered nonrestorable and should be extracted (see Figure 2).9,10
Patients who have been diagnosed with cracked tooth syndrome in more than one tooth should be counseled in strategies to prevent cracks in other teeth. These strategies may include discontinuing habits such as chewing ice and/or fabrication of a mouthguard.
When a clinician is unable to make a definitive diagnosis, the patient should be referred to a specialist who deals with these situations more frequently. Treatment should never be performed when a diagnosis cannot be made. Following this protocol will result in higher satisfaction for both patient and practitioner.
Prognosis
The sooner cracks are detected and treated, the more favorable the long-term prognosis. Epidemiologic data reveal that splits or fractures are the third most common cause of tooth loss in industrialized countries.2 This finding indicates that the cracked tooth syndrome is of high clinical importance. When at-risk teeth are treated early by complete cuspal coverage, the long-term prognosis is great. Furthermore, those symptomatic cases that receive root canal treatment and crowns before the crack propagates too far also have a favorable prognosis. ■
References:
1. Cameron CE. Cracked tooth syndrome. J Am Dent Assoc 1964; 68:930.
2. Lynch CD, McConnell RJ. The cracked tooth syndrome. J Can Dent Assoc Sept. 2002; 68(8):470-5.
3. Homewood CT. Cracked tooth syndrome-incidence, clinical findings and treatment. Aust Dent J Aug. 1998; 43(4):217-22.
4. Geurtsen W, Schwarze T, Gunay H. Diagnosis, therapy, and prevention of the cracked tooth syndrome. Quintessence Int. Jun. 2003; 34(6):409-17.
5. Clark DJ, Sheets CG, Paquette JM. Definitive diagnosis of early enamel and dentin cracks based on microscopic evaluation. J Esthet Restor Dent 2003; 15(7): 391-401.
6. Maxwell EH, Braly BV, Eakle WS. Incompletely fractured teeth: a survey of endodontists. Oral Surg Oral Med Oral Pathol 1986; 61:113.
7. Benenati FW. Coping with cracked tooth syndrome. J Okla Dent Assoc Winter 1996; 86(3): 16-8.
8. Kahler B, Moule A, Stenzel D. Bacterial contamination of cracks in symptomatic vital teeth. Aust Endod J Dec. 2001; 26(3):115-8.
9. Liu HH. Cracked teeth, treatment rationale and case management: case reports. Quintessence Int July 1995; 26(7):485-92.
10. Gutmann JL, Rakusin H. Endodontic and restorative management of incompletely fractured molar teeth. Int Endod J Nov 1994; 27(6):343-8.
Roxanne P. Benison, DMD
Dr. Benison received her DMD from Southern Illinois University School of Dental Medicine and her master’s in endodontics from Saint Louis University Center for Advanced Dental Education. She currently is in private practice in Edwardsville, Ill., and is on the adjunct faculty in endodontics at Saint Louis University.