Periodontitis, a global health crisis impacting up to half of the world's population,1 frequently goes unnoticed owing to its asymptomatic nature. To tackle this serious gum disease, researchers propose the adoption of an aMMP-8 rapid test, comparable to home pregnancy and COVID-19 antigen tests. Additionally, Finnish scientists have introduced a groundbreaking antibacterial, light-activated oral health enhancer designed for home use, with the potential to revolutionize oral care and plaque control.
Untreated periodontitis, impacting tooth-supporting tissues, heightens the body’s chronic low-grade systemic inflammation, linking it to diseases like diabetes, cardiovascular issues, Alzheimer’s disease, and even pancreatic cancer. Low-grade systemic inflammation is a condition in which the body responds to irritation by releasing mediators. The sustained inflammation this causes, while considered “mild,” can become harmful to the body over time.2-4
Individuals with periodontitis may even have a higher risk of developing serious forms of cancer. According to an analysis published in the British Journal of Cancer, individuals aged 50–70 with periodontitis had a 20% higher likelihood of developing pancreatic cancer compared to participants with healthy gums. The risk of developing cancer was also elevated in patients who had already lost several teeth, indicating advanced periodontitis.5
The study utilized registry data encompassing nearly 6 million individuals aged 19 and older residing in Sweden. Over a seven-year follow-up period, 10,000 of these individuals were diagnosed with pancreatic cancer.5
Hidden periodontitis uncovered?
Periodontitis is an inflammatory-infectious disease that causes collagen fibers attaching teeth to the jawbone to break. In severe cases, teeth may loosen or even detach. Early signs of periodontitis include red gums, bleeding gums, and bad breath.1,2
“In Finland, more than 10% of the population has severe periodontitis in their mouths. In such cases, the inflamed area around the tooth’s supporting tissues can be as large as the palm of a hand. Even in milder cases, there is an inflamed ‘wound surface’ causing low-grade systemic inflammation in the body,” explains heart and transplant surgeon and researcher Dr. Tommi Pätilä from the HUS Hospital in Helsinki, Finland.
Given the association between periodontitis and various systemic diseases, the timely detection and treatment of this condition are paramount for overall well-being. Researchers have now developed an effective method to address this critical aspect.
Matrix metalloproteinase-8 is primarily an enzyme produced by human white blood cells, or neutrophils, and its role is to enable collagenolytic neutrophils’ passage to the inflamed area by modifying the extracellular matrix. In patients with periodontitis, the aMMP-8 enzyme becomes catalytically active and tissue-destructive due to its abundant presence.6,7
According to Professor Timo Sorsa of the University of Helsinki’s Department of Oral and Maxillofacial Diseases, using the aMMP-8 chairside test can measure and assess active and progressive attachment loss within five minutes, directly in the dentist’s chair and noninvasively. The test complements the diagnostics of periodontitis and peri-implantitis, monitors treatment outcomes, and supports maintenance therapy.6,7
A tool against systemic diseases
Professor Sorsa says that aMMP-8 tests measuring the activity of periodontal and peri-implant diseases differentiate between diseased and healthy tissues with accuracy. In patient care, a negative result in the aMMP-8 test is the aim. This indicates healthy tissue with a low risk of attachment loss and its progression, and it can also be regarded as a biomarker of periodontal health.
The current oral health treatment protocol could be significantly enhanced by incorporating the developing aMMP-8 rapid test, which can conveniently identify not only periodontitis but also diabetes and its precursors based on oral enzymes. The aMMP-8 enzyme test can also accelerate the diagnosis of gum diseases in patients before dental implant surgery. While traditional methods involve culturing problematic bacteria in laboratories, which takes days to weeks, the aMMP-8 test provides a quicker alternative for identifying issues before implant placement.8
Professor Sorsa says, “Results from the aMMP-8 enzyme test can be obtained within five minutes of conducting the test. Research results are already promising regarding the functionality of the test, and a test of this kind could be in common use within the next five years.”
Effective and swift diagnostics, screening, and treatment of periodontitis can positively influence the outcomes of diabetes treatment, too, potentially leading to a reduction in treatment costs. Diabetes screening and successful treatment not only decelerate the progression of periodontitis but also contribute to diminishing the associated treatment expenses.
Eliminating problem-causing bacteria
In addition to rapid diagnosis, there is a pressing need for more effective methods to eliminate problem-causing bacteria from the oral cavity. Research indicates that 95% of all oral diseases are attributed to plaque. The harmful bacteria present in plaque can escalate the risk of severe conditions like heart attacks and diabetes and even contribute to the development of serious cancer types.9 Research shows that merely brushing teeth is insufficient to eradicate these detrimental bacteria.10
Ing-Marie Albinsson, a dental hygienist at the Lilla Tandkronan clinic in Arvika, Sweden, says, “Mechanical brushing is a very important step that removes about 65% of the plaque, so we absolutely need to continue doing it regularly. But to really get rid of all the harmful bacteria from the mouth, a complement is needed.”
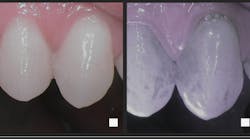
For this reason, Finnish researchers developed an antibacterial and light-activated device (Lumoral; not yet available in the United States) that targets dental plaque and eliminates harmful bacteria from the mouth. The method has earned endorsement from the Finnish Association of Oral Hygienists and is designed for home use. It serves as a complementary tool to conventional oral hygiene practices such as brushing and flossing.10-12
Dr. Pätilä, founder of Koite Health (the Finnish company that developed this groundbreaking technology) and one of the key scientists behind the development of the device, says, “I have performed surgeries on numerous patients, and in many instances observed that oral bacteria were responsible for causing heart problems. However, a pivotal moment occurred around a decade ago when I operated on a child suffering from a severe heart infection directly attributable to oral bacteria. It was at that point I realized that sufficient action was necessary to improve the oral health of both adults and children.” He stresses that the tricky thing about oral infections is that they often have no symptoms. If dental plaque is not removed thoroughly, bacteria can pass through the gums into the bloodstream.
Preventing the spread of bacteria
How can you prevent bacteria from passing through the gums into the bloodstream? The first step is brushing and flossing (or using interdental brushes), but going a step further and adding regular antibacterial dual-light treatment is an ideal complement, especially for those with periodontal issues. Antibacterial photodynamic therapy hampers plaque formation and significantly reduces the number of periodontal bacteria in the mouth.12-14
Preliminary observations suggest that antibacterial dual-light therapy might even be an important tool in the armamentarium for oral mucositis treatment in patients undergoing cancer treatments, particularly radiation and chemotherapy. To date, no existing medication has effectively prevented the development of oral mucositis, but recent research suggests antibacterial dual-light therapy may be an effective method to manage the symptoms of this condition.
A new doctoral dissertation study will commence at the University of Helsinki in the spring to delve further into this topic.
Editor’s note: This article first appeared in Clinical Insights newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe.
References
- Nazir M, Al-Ansari A, Al-Khalifa K, Alhareky M, Gaffar B, Almas K. Global prevalence of periodontal disease and lack of its surveillance. ScientificWorldJournal. 2020;2020:2146160. doi:10.1155/2020/2146160
- Cecoro G, Annunziata M, Iuorio MT, Nastri L, Guida L. Periodontitis, low-grade inflammation and systemic health: a scoping review. Medicina (Kaunas). 2020;56(6):272. doi:10.3390/medicina56060272
- Petersen PE, Baehni PC. Periodontal health and global public health. Periodontol 2000. 2012;60(1):7-14. doi:10.1111/j.1600-0757.2012.00452.x
- Bartold PM, Van Dyke TE. Periodontitis: a host-mediated disruption of microbial homeostasis. unlearning learned concepts. Periodontol 2000. 2013;62(1):203-217. doi:10.1111/j.1600-0757.2012.00450.x
- Yu J, Ploner A, Chen MS, Zhang J, Sandborgh-Englund G, Ye W. Poor dental health and risk of pancreatic cancer: a nationwide registry-based cohort study in Sweden, 2009–2016. Br J Cancer. 2022;127(12):2133-2140. doi:10.1038/s41416-022-02018-8
- Sorsa T, Alassiri S, Grigoriadis A, et al. Active MMP-8 (aMMP-8) as a grading and staging biomarker in the periodontitis classification. Diagnostics (Basel). 2020;10(2):61. doi:10.3390/diagnostics10020061
- Öztürk VÖ, Emingil G, Umeizudike K, et al. Evaluation of active matrix metalloproteinase-8 (aMMP-8) chair-side test as a diagnostic biomarker in the staging of periodontal diseases. Arch Oral Biol. 2021;124:104955. doi:10.1016/j.archoralbio.2020.104955
- Lähteenmäki H, Räisänen IT, Pärnänen P, Tervahartiala T, Sorsa T. aMMP-8 enzyme test and dental implants. Suomen hammaslääkärilehti. 2021;28(11):32-39.
- Gupta S, Räisänen IT, Seppänen H, et al. aMMP-8 POCT for periodontal disease: an indicator of poor oral health. Cancer Control. 2023;30:10732748231214874. doi:10.1177/10732748231214874
- Aggarwal N, Gupta S, Grover R, Sadana G, Bansal K. Plaque removal efficacy of different toothbrushes: a comparative study. Int J Clin Pediatr Dent. 2019;12(5):385-390. doi:10.5005/jp-journals-10005-1669
- The Finnish Oral Hygiene Association recommends Lumoral. Finnish Association of Dental Hygienists. September 1, 2022. https://www.suuhygienistiliitto.fi/suomen-suuhygienistiliitto-suosittelee-lumoralia/
- Trujillo K, Räisänen IT, Sorsa T, Pätilä T. Repeated daily use of dual-light antibacterial photodynamic therapy in periodontal disease—a case report. Dent J (Basel). 2022;10(9):163. doi:10.3390/dj10090163
- Pakarinen S, Saarela RKT, Välimaa H, et al. Home-applied dual-light photodynamic therapy in the treatment of stable chronic periodontitis (HOPE-CP)—three-month interim results. Dent J (Basel). 2022;10(11):206. doi:10.3390/dj10110206
- Gholami L, Shahabi S, Jazaeri M, Hadilou M, Fekrazad R. Clinical applications of antimicrobial photodynamic therapy in dentistry. Front Microbiol. 2023;13:1020995. doi:10.3389/fmicb.2022.1020995
Nina Garlo-Melkas, MSc, is a health and science journalist who works as communications manager at Koite Health Ltd., a quickly growing health technology company and innovator in light-activated antibacterial solutions for treating and preventing oral diseases.