The dos and don’ts of death: Interacting with grieving patients
Sometimes, patients may confide in us about the death of a loved one. It is important to remain professional while responding kindly, as we all want to do. Following are several things to remember when a grieving patient sits in your chair.
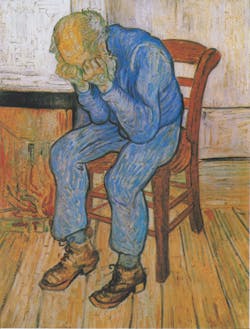
Sorrowing Old Man (At Eternity's Gate), Vincent Van Gogh, 1890. Wikimedia Commons.
For years, those dealing with the loss of a loved one would be given therapeutic feedback from the framework of the five stages of grief that were first presented in the book On Death and Dying, by Elisabeth Kübler-Ross, written in 1969. During that time, practitioners had limited data and research for comparison. They used those stages in their grief counseling because of the predictability and sense of manageability it gave them in their practice. In 2000, the founder of the Center for Advancing Health, Jessie Gruman, BA, PhD, was given a grant as part of the Project on Death in America, funded by a nonprofit called the Open Society Institute, to update grief research. In her report, Dr. Gruman stated that grief is not a series of steps, rather a set of symptoms that come and go and “eventually, simply lift.” (1)
What does this mean for the dental team that has patients who have suffered the loss of a loved one? Don’t tell them they are going through the stages of grief; each experience is individualized and research demonstrates this.
RECOMMENDED: Saying goodbye to a dying patient
Grief counseling has not shown to be more effective than the passing of time in those with a “normative response.” (2)This is not to discount counseling, but it demonstrates that grief lets up when an individual is ready under normal circumstances.
We are not trained psychologists, but like in many customer service industries, patients often reveal their trauma to us, and most especially when we have had a rapport built for years. If you are not sure how you should respond to death, don’t force it or think you need to know the proper thing to say. Nine times out of 10, we are better off lending an ear—and that’s it.
Don’t: Share your own experience with a loss. This is the patient’s time, and he or she needs it, even if you think you know how they feel. Can it help? Maybe, but why try if you are uncertain?
Do: Respect the patient’s time. Offer an ear, empathy, and compassion. Listen if the patient would like to share. Be prepared to run over your appointment time.
Don’t: Give them a random name of a therapist you googled, and certainly not your own therapist. This could work against you if the patient doesn’t have a good experience.
Do: Have information on community bereavement groups. They are much better for those who are experiencing grief, because a group of others who have all experienced a loss offers more comfort than someone who has never suffered through that experience. (3, 4)
Don’t: Review their treatment plan and remind them of the work they need.
Do: Give them a break or pass on their oral health that day! Unless the patient has an abscess or infection that is detrimental to his life, leave him alone.
Don’t: Watch the patient cry and wipe her eyes and nose with her shirt. It may appear rude to get up while the patient is crying, but politely excuse yourself and grab the tissues.
Do: Have a tissue box handy to avoid the above.
Don’t: Discount the person who lost his pet, and breaks down like you would if it were your child.
Do: Respect any loss that upsets someone, and his or her view of it as a tragedy.
Don’t: Bring up the loss if the patient did not tell you.
Do: Let the patient share if they choose. There are times when we have had a rapport with a patient for a long time, and we feel we must offer something, a gentle touch or hug. This is OK if you know the patient. Sometimes people do not want to talk about it. Yet when we have seen them for so many years, how can we not express sympathy? Gently touch the patient’s arm and say, “I am so sorry for your loss.”
Don’t: Tell everyone in the office about what you have learned.
Do: Respect the patient’s privacy in this matter. Sometimes others will take it upon themselves to mention this to the patient, and then it may appear as if you violated the confidentiality the patient had in you.
Don’t: Send a gift certificate to your office or any irrelevant monetary gift card.
Do: Send a card or a note of sympathy. Also, if your office knows that services will be held, send flowers. Whatever it may be, it should be culturally appropriate.
Don’t: Make a note in any part of the chart the patient may see, or that can’t be erased, that details your conversation with the patient and puts shame on their temporary oral health status. If the patient ever decides to request her records, she may have resentment toward you for writing this down.
Do: Make a note in the chart that the patient has experienced a loss of a loved one and oral health may be compromised.
Don’t: Feel as if you need to tell the patient that his oral health is poor and you just want to help him; he probably knows.
Do: Be prepared to notice a decline in oral or overall health. Make yourself a note to follow up with the patient at his next recare in a calendar, or set a reminder in your computer.
Don’t: Call the patient who missed her next appointment and berate her.
Do: Call to check up on the patient if she has not been back for her regularly scheduled recare. At that time, you can also say something like, “We are here if you need anything. May I please follow up again in a few weeks if I notice an appointment has not been scheduled?” Always ask for permission.
Don’t: Be unprepared in interacting with patients who have recently lost a loved one.
Do: Have a meeting in the office and discuss what to do when this happens. If someone in your office has found out a patient coming in that day has lost someone, review it in your morning huddle. Discuss the possibility of running over the appointed time and make arrangements for someone else to offer assistance for your next patient.
Editor's note: This article first appeared in RDH eVillage. Click here to subscribe.
References
1.Genevro JL, Marshall T, Miller T, Center for the Advancement of Health. Report on bereavement and grief research. Death Stud. 2004;28(6):491-575. doi: 10.1080/07481180490461188.
2. Bonanno GA, Boenrer K. The stage theory of grief. JAMA. 2007;297(24):2693. doi: 10.1001/jama.297.24.2693-a.
3. Knight C, Gitterman A. Group work with bereaved individuals: The power of mutual aid. Soc Work. 2014;59(1):5-12. doi: 10.1093/sw/swt050.
4. Barrett CJ. Effectiveness of widows' groups in facilitating change. J Consult Clin Psychol. 1978;46:20-31.
Elicia Lupoli, RDH, BSDH, is on the editorial board for RDH magazine and Hygienetown, as well as an editor for her state association’s quarterly newsletter (ADHA Connecticut). Elicia attributes the start of her writing career to Shirley Gutkowski, RDH, BSDH, and other success to her many mentors.