Originally published on January 31, 2017. Updated April 23, 2021.
Is the tooth cracked or fractured? Does it need a root canal? You’ll want to keep the decision matrix in this article as a reference tool for your endo cases.
Resource for your patients >>> Cracked tooth: Types, causes, and treatments
Patient: “My tooth hurts, especially when I bite down.”
You: “Does the pain linger? Is it sensitive to hot and/or cold? How long has the pain been going on?”
Meanwhile … tests begin and clues to the puzzle begin to come together.
Diagnosis: Cracked tooth? Fractured tooth? Split tooth? Extent—unknown (or … you may have an idea, but it is subjective). So how do you decide which one it is?
Now what? Root canal? Crown? What is the prognosis for treatment versus alternative replacement options? These are all questions that run through my mind when a patient presents with a cracked or fractured tooth. Sure, the test results will dictate a subsequent recommended treatment plan; however, what I’ve learned is that there is not a one-size-fits-all diagnosis and treatment for teeth such as these. Why is that?
Additionally, one must consider patients who present with completely asymptomatic craze and crack lines all over their teeth. You cringe just looking at these teeth and know that there’s likely going to be a problem at some point down the road. What is the dialogue that you have with these patients? “Watch” these teeth? Recommend crowns (and often get accused of trying to bamboozle money from the patient for expensive dental work because a second opinion from another dentist suddenly renders you incompetent)? The conundrum is real.
ALSO BY DR. GIVIDEN | Endodontics reference guide: Distinguishing differences between internal and external resorption
Treatment and outcome for a cracked or fractured tooth is dependent on location, direction, type, and size of the crack.1 Being able distinguish the difference can aid in a diagnosis that will ultimately lead to proper care and treatment.
The American Association of Endodontists has classified five types of cracks in teeth:2,3,6
- Craze lines (figures 1 and 2)
- Fractured cusp (figure 3)
- Cracked tooth (figure 4)
- Split tooth (figures 5 and 6)
- Vertical fracture
With the exception of craze lines, all types are typically found in the posterior teeth, and unlike bone, cracks/fractures in a tooth will never heal.4
ALSO BY DR. GIVIDEN | Clinical blunders, mishaps, and picking the right kind of irrigant when doing root canal therapy
Several tests can be done to help confirm a diagnosis:4-7
- Dental history—Restoration assessment, habits (chewing/biting, clenching, grinding, etc.), when the symptoms started occurring (i.e., what the patient bit down on when it started hurting)
- Clinical/visual examination—Observation of wear facets, noting defects and location of the crack(s)
- Tactile examination—Can you catch the tip of an explorer over the surface of the tooth where the crack is?
- Periapical/percussion tests—To assess the presence of inflammation in the periodontal ligament
- Bite tests—Used to try to mimic the patient’s symptoms; can be done simply with a cotton roll. If the patient bites and then has a sharp pain upon release, the diagnosis is confirmed. Isolating the culprit cusp with a tooth sleuth or other similar tool aids in comprehensive assessment and treatment planning.
- Vitality testing—Usually positive, but not always. Hypersensitivity is not uncommon due to pulpal inflammation.
- Periodontal probing—Look for probing patterns and the presence of inflammation. Can be especially helpful when diagnosing vertical root fractures.
- Radiographic examination—It is rare to see a crack on a radiograph, but bone resorption and periodontal/pulpal health can be observed.
- Restoration removal—Cracks are commonly observed running in a mesiodistal direction underneath old restorations
- Staining, transillumination, wedging forces, and surgical assessments
A summary table, taken from Walton and Torabenejad is referenced below, with some modifications by the author. Note: Since craze lines are for the most part benign, they are not included in the table, but summary points are given for reference.
Craze lines
- Most benign; visible fractures that only involve enamel
- Most adult teeth have craze lines; in the “posterior, they are usually evident crossing marginal ridges and extending along buccal and lingual surfaces”5
- Craze lines in the anterior are long and typically affect the enamel; are painless and of no concern beyond esthetics
- Occur naturally; increase in incidence with restorations or injury
- Challenge: It’s not always possible to tell if the fracture is limited to the enamel
Case report No. 1
A healthy 55-year-old male presented with the chief complaint that his gum tissue on the upper right side had been hurting for the last few months. He thought something was stuck in the tissue and had unsuccessfully “tried to pick out whatever was stuck in there.” He pointed to the area around tooth No. 3.
A radiograph assessment revealed a slight radiolucency at the apex of the palatal root on tooth No. 3 (figure 8). Biting and percussion was WNL; probing depths were 6 mm interproximal and 3–4 mm on the facial/lingual. Cold and electric pulp tests were negative. The vestibular area in the No. 3–4 area was tender to palpation. Clinically, a large fracture line was noted on the lingual and on the distal marginal ridge (figure 9).
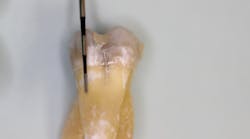
Diagnosis: Necrotic No. 3 with likely association of extended fracture line into the pulpal space. Recommendations were given to the patient, who opted for extraction and eventual implant placement. Upon removal of the tooth, the following was noted (figure 10):
- Lingual fracture line extending approximately 5 mm below the CEJ
- Existing restoration was removed and the crack line was observed to run across the pulpal floor in a mesiodistal fashion
- Wedging was done, and there was a noted flexuration in the cusps
Case report No. 2
A 72-year-old male presented for a comprehensive exam with a chief complaint that the tooth on the upper right side had had a root canal done twice, but he was still in pain. He was wondering if there was a possible sinus infection. Health history included a pacemaker, Warfarin, and thyroid cancer.
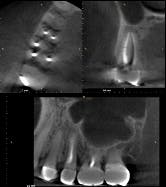
Testing of the upper right side was, for the most part, inconclusive, aside from some 6 mm pockets in the upper right quadrant. Radiograph was WNL (figure 11). A potential sinus infection was discussed, along with the possibility of a periodontal abscess. The patient was placed on antibiotics, referred to an ENT, and had scaling and root planing done on the upper right quadrant.
The report from the ENT was negative. The symptoms persisted and, in fact, started to worsen. The likelihood of a vertical root fracture was then discussed with the patient. He was referred to an endodontist who took a CBCT scan.
Evaluation by the endodontist showed a very small direct, vertical 9 mm drop on the lingual with radiolucency on the lingual root in the scan about halfway down (figure 12). Given the history of the double root canal, symptoms, and radiographic evidence, it was concluded that the patient had sustained a vertical root fracture on the lingual root of tooth No. 4. Prognosis was poor, and the tooth was removed with discussion regarding replacement options.
This case is a classic example of how elusive diagnosing these types of teeth can be and how critical a comprehensive assessment is to produce the most accurate diagnosis.
Editor’s note: The CBCT scan in case No. 2 (figure 12) is courtesy of Joseph A. Petrino, DDS, MS; Missoula, Montana.
References
1. Paul RA, Tamse A, Rosenberg E. Cracked and broken teeth—definitions, differential diagnosis and treatment. Refaut Hapeh Vehashinayim. (1993). 2007;24(2):7-12, 68.
2. Hasan S, Singh K, Salati N. Cracked tooth syndrome: Overview of literature. Int J Appl Basic Med Res. 2015;5(3):164–168. doi: 10.4103/2229-516X.165376.
3. Lubisich EB, Hilton TJ, Ferracane J. Cracked Teeth: A review of the literature. J Esthet Restor Dent. 2010;22(3):1-11.
4. American Association of Endodontists: Cracked teeth. http://www.aae.org/patients/symptoms/cracked-teeth.aspx. Accessed January 19, 2017.
5. Rivera E, Walton RE. Cracking the cracked tooth code: Detection and treatment of various longitudinal tooth fractures. In: Endodontics: Colleagues for Excellence newsletter. American Association of Endodontists; Summer 2008:1-8.
6. Mathew S, Thangavel B, Mathew CA, Kailasam S, Kumaravadivel K, Das A. Diagnosis of cracked tooth syndrome. J Pharm Bioallied Sci. 2012;4(Suppl 2):S242–S244. doi: 10.4103/0975-7406.100219.
7. Walton RE, Torabinejad M. Principles and practice of endodontics. 2nd ed. Philadelphia, PA: WB Saunders Company; 1996:474-492.
Stacey L. Gividen, DDS, a graduate of Marquette University School of Dentistry, is in private practice in Hamilton, Montana. She is a guest lecturer at the University of Montana in the Anatomy and Physiology Department. Dr. Gividen is the editorial co-director of Through the Loupes and a contributing author for DentistryIQ, Perio-Implant Advisory, and Dental Economics. She serves on the Dental Economics editorial advisory board. You may contact her at [email protected].