You may know that June is Alzheimer’s and Brain Awareness Month. As hygienists, we are coming in contact with more and more dementia patients. Unless some close to us has suffered dementia, we may not really understand the whole spectrum of the disease. This article will focus on simple, practical considerations you can incorporate into your practice when you care for these patients.
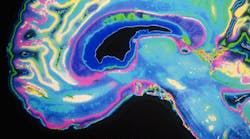
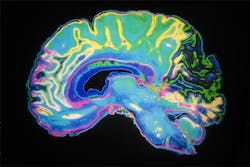
Disease overview
There are several types and degrees of dementia. The Alzheimer’s Association lists 10 different types. The most common is Alzheimer’s disease. The second most common is vascular dementia, which occurs after stroke. Vascular dementia accounts for 10% of dementia cases. Alzheimer’s disease can be sneaky in that it may be present for several years; the patient and family members often do not recognize it until the “moderate” stages.
With Alzheimer’s disease, the patient can live 20 years or more depending on the amount of brain tissue that is affected by amyloid lesions. Vascular dementia patients usually live up to three years. If you have some time, please look at the Alzheimer’s Association website for insight on specific types of dementia to educate yourself and others.
So how can we as hygienists help our patients in their fight against the disease?
READ MORE | Perisolv: A new way to treat perio using bleach
Patience is paramount
One of the biggest ways in which we can help is to practice extra patience and understanding in our interactions with the patients and their caregivers. This is the absolutely fundamental, but it is not always adhered to. As providers, we are challenged to take ourselves out of the picture and really focus on the patient in front of us.
Keep in mind that dementia patients are on edge and your nonverbal actions may frighten them. Sudden movements, such as draping them with a lead apron without explanation of what’s happening first, should be avoided. Humanity needs to be heighten a little with a dash of going above the bar to care for these patients. They are truly living in their own world. Interacting with a dementia patient heightens your awareness of the disease. Of course there are hygiene tips we will address, but the first line of action is to genuinely care for people and their situations—everyone is carrying more than any of us know.
Cognitive considerations
Dental hygiene considerations for dementia patients are not black and white. We wish there was a protocol that could be followed to a T, but we are dealing with layers of disease levels and progressions. Assessment of the patient’s cognitive level every time you see them can be extremely tricky. We are not there to give them a neurological exam, but in order for us to give patient education and also explain diagnosis and treatment plans, having an understanding of the patient’s cognitive state will help. This is where the caregiver, if the patient has one, comes in hand. When talking with a caregiver, remember that the patient can sometimes feel left out. Please include the patient as much as possible; even though they may not be power of attorney for themselves, they very well know the conversation is about them.
Short-term memory loss is a huge component to dementia. During the visit, they may not remember their list of medications, for example. They may repeat themselves or ask the same question again and again. Write down home care instructions and product recommendations. My grandmother called me after her doctor’s appointment and said that she forgot the name of the over-the-counter vitamin for memory that the doctor told her to take for memory loss.
READ MORE | True story: My physician asked me about my oral health
Also, it is good to know that mood change is something that comes with dementia. Your patient that you have seen for years may suddenly not know who you are and their personality may also be totally different. They may seem distant one visit and on cloud nine another. Do not take this personally. It is just the disease and not aimed at all towards the provider.
Usually you can safely see dementia patients in the early, mild, and early moderate stages. When the disease progresses into the moderate to severe stage, the patients will most likely not be able to come into the office and will be taken care of by a caregiver at home or in a facility. This is where any information you have previously given to the caregiver would come in. If the patient has not been to the office in a while, a hand-written note is always nice, as well as a sheet of home care tips for dementia patients for the caregiver.
Making the appointment run smoothly
Prophy appointments should be individualized. The patient might have developed a new fear or apprehension. While bringing the patient back, remember that they might walk slow or shuffle; don’t race ahead of them. Talk to them as you walk them into the room. Communicate with them always so they always feel comfortable. Give patient education, as always, with a few written tips. Repeat these tips multiple times throughout the appointment while working on the patient. Ask their preference on flavor of prophy paste. Their taste perception might have change.
If they have vascular dementia, which occurs after stroke, they may have difficulty swallowing, making the ultrasonic challenging. Consider having an assistant for superior suctioning. You may not be able to use an ultrasonic scaler on dementia patients at an increased risk of aspiration.
If there is a caregiver with the patient, make sure to recap any recommendations so that someone can follow up for the patient if needed. Appointment times should be kept as short possible to make the patient more comfortable. Recall appointments should always be written down; reminders should be sent a week and then a day before. Frequent recare appointments may be necessary when their home-care measures are failing. If a caregiver brings them to the appointment, try to get their phone number for reminders.
Conclusion
We hope that you find these tips useful. We have focused on tips to help our fellow hygienists understand the disease. Also, we wanted to share a little insight on the patient’s view of the disease, as Nicole’s father passed away from vascular dementia and her grandfather currently has moderate dementia. Jackie’s grandmother passed away from Alzheimer’s disease and her mother is currently battling the same. The devastation of this disease and the rapid increase in cases means that our profession and others need to be aware and have an understanding of how to treat the patients successfully and help raise the bar to a best practice care.