Familial cancer risk assessment: Breast and ovarian cancer
This article will review hereditary breast and ovarian cancer, genetic counseling, and testing for hereditary breast and ovarian cancer, cancer family history, and when one should be referred for genetic services.
Incidence
5–10% of breast cancers have a strong hereditary component. 15–20% are “familial” or multifactorial, and 70–75% are thought to be sporadic.1 Hereditary breast or ovarian cancers occur in multiple generations. Some of the presentations are younger ages of onset (often <50), bilateral cancer or multiple primaries, and a family history of unique tumor combinations.1
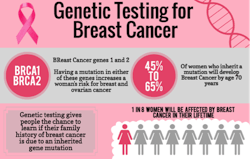
5–10% of all cases of breast and ovarian cancer are hereditary. Approximately 70–85% of these hereditary cases are caused by mutations in either the BRCA1 or BRCA2 gene. Genetic testing for BRCA1 and BRCA2 gene mutations is accessible to women with a family history meeting “hereditary breast cancer” criteria. BRCA1/2 mutations occur 1 in 800 women in the general population, and 5–10% of all women with breast cancer. 2% of all women of Ashkenazi Jewish ancestry are at risk.1 Other hereditary breast cancer syndromes include Cowden syndrome (less than 1% of all cases), Li-Fraumeni syndrome (less than 1% of all cases), and Peutz-Jeghers syndrome (than 1% of all cases).
Click on the image to view a full version of the infographic.
Genetic counseling considerations
Genetic counseling for cancer risk involves full pedigree analysis and risk assessment. The counselor will ask about and discuss personal risks of cancer based on family history; risks of genetic syndrome in the family; applicable genetic testing and chances of mutation; full informed consent prior to genetic testing; personalized, risk-based screening and prevention options; and support resources.
There are a number of ethical issues to be considered. Confidentiality and privacy are paramount, as well as protecting family members’ confidentiality when documenting family history. Potential insurance, employment, and social discrimination issues must be taken in account, as well as sharing information with at-risk relatives.
Risk assessment tools
The former Gail model is now called The Breast Cancer Risk Assessment Tool. It is an interactive instrument designed by scientists at the National Cancer Institute (NCI) and the National Surgical Adjuvant Breast and Bowel Project (NSABP) to estimate a woman's risk of developing invasive breast cancer. The Breast Cancer Risk Assessment Tool is based on a statistical model known as the Gail model, which is named after Dr. Mitchell Gail, senior investigator in the Biostatistics Branch of NCI's Division of Cancer Epidemiology and Genetics.2 The model uses a woman's own personal medical history, her own reproductive history, and the history of breast cancer among her first-degree relatives (e.g., mother, sisters, daughters) to estimate her risk of developing invasive breast cancer over specific periods of time.2
The Claus model was developed by Claus and colleagues as a risk model for familial risk of breast cancer in a large population-based, case-control study conducted by the Centers for Disease Control.3 The chief disadvantage of the Claus model is that it does not include any of the nonhereditary risk factors.
The Myriad Risk Tables identify the chance of detecting a BRCA1 or BRCA2 mutation in women with a family history of early-onset breast and/or breast and ovarian cancer. The BRCA Risk Calculator is based on data, updated periodically, that represent observations of harmful mutations by Myriad Genetic Laboratories through its clinical testing service. The data on Ashkenazi Jewish ancestry are for patients tested for the three prevalent founder mutations and for patients tested by full sequence analysis. The method used to develop the prevalence tables has been published.4
For more information about BRCA1 and BRCA2, and other genes associated with breast cancer, visit breastcancer.org. Thereare also fact sheets available from the National Cancer Institute, the National Health Service of the UK, and the National Institutes of Health.
Editor's note: This article was originally published in 2015 and has been updated as of June 2025.
References
1. Genetics. Breastcancer.org. http://www.breastcancer.org/risk/factors/genetics. Accessed November 3, 2015.
2. About the Gail Model. National Cancer Institute. http://www.cancer.gov/bcrisktool/about-tool.aspx#gail. Accessed November 3, 2015.
3. Evans DGR, Howell A. Breast cancer risk-assessment models. Breast Cancer Research. 2007;9:213. doi:10.1186/bcr1750. http://www.breast-cancer-research.com/content/9/5/213.
4. Frank TS, Deffenbaugh AM, Reid JE, et al. Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: Analysis of 10,000 individuals. J Clin Oncol. 2002;20(6):1480-1490.