According to Medscape, “anaphylaxis is an acute, possibly fatal, multiorgan system response caused by the release of chemical mediators from mast cells and basophils.” (1) Rapid intervention is essential. This article will discuss prevention, recognition, and treatment of this condition.
Practice parameters recently released by the American Academy of Allergy, Asthma and Immunology; the American College of Allergy, Asthma and Immunology; and the Joint Council of Allergy Asthma and Immunology recommend that patients with signs of anaphylaxis should receive epinephrine in the anterolateral thigh as first-line treatment in the emergency department. (2) The report was published in December 2014. The practice parameters also recommend a number of other protocols for diagnosing and treating anaphylaxis. Clinical symptoms are usually sufficient to produce a diagnosis; however, if the diagnosis is not clear, laboratory tests can be performed. Anaphylaxis is a medical emergency and requires immediate intervention, management, and pharmacotherapy.
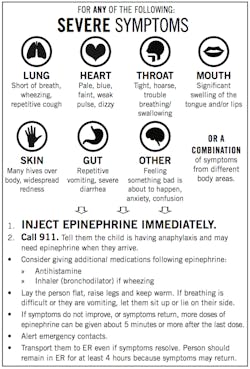
It is important to recognize signs of anaphylaxis. Most people have a combination of urticarial (hives), erythema, pruritus, or angioedema (sudden swelling). (3) Children tend to have more respiratory symptoms (e.g., nasal congestion, sneezing, inflammation of the nasal mucous membrane). Shortness of breath, wheezing, flushing, palpitations, dizziness, and blurred vision are all signs that should cause concern. For complete signs and symptoms, visit the Mayo Clinic or the American Academy of Allergy, Asthma, and Immunology websites.
RECOMMENDED BY THE AUTHOR |Allergic reactions to dental materials, drugs require an alert response from practitioner
Food reactions
In addition to insect bites, pharmaceuticals, latex, and other triggers, certain foods are culprits in severe allergic reactions. Peanut allergy is a prime example. It is important to educate patients, their caregivers, and those at risk to avoid foods or situations that might trigger an allergic reaction. The Food Allergy & Anaphylaxis Network (FARE) is an excellent resource. FARE supports the 15 million Americans with food allergies, including all those at risk for life-threatening anaphylaxis. This conceivably deadly disease affects 1 in 13 children in the United States, or approximately two in every classroom. (4) The International Food Allergy & Anaphylaxis Alliance is an association of 11 global patient education groups. (7) Their mission is to unite organizations involved in food allergy and anaphylaxis to exchange information and report important issues to those with food allergies and anaphylaxis. Click here for a Food Allergy Guide, a packet for individuals and families who have been newly diagnosed with food allergies.
There are many other resources available, such as the fact sheet, “Tips for Avoiding Your Allergen.” (9) The Be a PAL: Protect a Life program for parents, teachers, scout troop leaders, youth group leaders, or coaches also offers several resources here.
Anaphylaxis is a very serious situation, so it is vital to recognize the symptoms. Auto-injectable epinephrine (also know as adrenaline) should be given early in the reaction in an attempt to halt or delay the condition from getting worse. People with a severe allergy or a history of anaphylaxis should carry epinephrine with them at all times. Being prepared for an emergency is essential, and those with allergies should consult with their medical professional to identify allergens that trigger symptoms. Avoidance of these allergens is critical, as is an action plan for emergency situations. It is important for the person with severe allergies and health care professionals to be able to administer epinephrine on themselves or others if needed. Keep epinephrine close by at all times for emergency use.
RECOMMENDED BY THE AUTHOR |Medical emergencies in dentistry: Prevention and preparation
Be prepared!
References
1. Mustafa SS. Anaphylaxis. Medscape. http://emedicine.medscape.com/article/135065-overview. Accessed May 11, 2015.
2. Campbell RL, Li JT, Nicklas RA, Sadosty AT. Emergency department diagnosis and treatment of anaphylaxis: a practice parameter. Ann Allergy Asthma Immunol. 2014;113:599-608.
3. Webb LM, Lieberman P. Anaphylaxis: a review of 601 cases. Ann Allergy Asthma Immunol. 2006; 97:39-43.
4. Home page. Food Allergy Research & Education. http://www.foodallergy.org/. Accessed May 11, 2015.