This article first appeared in the newsletter, DE's Breakthrough Clinical with Stacey Simmons, DDS. Subscribe here.
In the hectic, modern world, most of us witness annoying behaviors that get under our skin on a daily basis. I think of myself as an easy-going guy, but when thinking about things that are irksome to me, I am able to come up with a surprisingly long list. I am irritated by the person sitting next to me on a cross-country, red-eye airline flight who wants to make small talk, when all I can think about is sleep. It is maddening that the slowest car on the road insists on driving in the fast lane during the busy, morning rush hour. For the sake of brevity, I won’t list anymore day-to-day annoyances, but I would like to focus on a statement that I hear with some frequency in my clinical practice or at continuing education events that I attend. I have to compose myself when I hear a fellow clinician make the statement: “I only do root canals on incisors and premolars. I refer out the molar teeth, because I only like to treat the easy ones.” I have thought about this statement on many occasions, and there are three reasons why it is bothersome to me.
1. No teeth are easy.
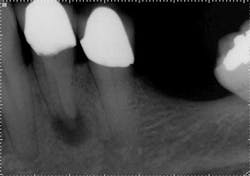
The success of endodontic treatment is directly related to the clinician’s ability to remove maximum numbers of bacteria from the root canal system. (1,2) If we can agree that all root canal treatment is associated with a certain degree of skill and precision in spite of perceived ease of treatment, I think it is fair to say there are no easy root canals. Some teeth are more difficult than others due to access limitations or anatomy, but the problem that faces all of us, in every tooth, is our inability to measure the absence of bacteria within the root canal and the potential for microanatomy to exist at any level of the root—whether it is a five-canal molar or a single-rooted anterior. It is impossible to determine the exact terminus of the root canal system, and there is no uniform agreement about where the root canal system ends. (3,4) The use of an apex locator can aid in this determination, but there is often disagreement between radiographic information and an apex locator, even in single-rooted anterior teeth, because the canal terminus can be at the radiographic apex or as much as 3 mm from it. (5) All instrumentation techniques leave a certain amount of the canal wall untouched, and we are not able to sterilize the root canal system. (6,7) The apical portion of any tooth may have dentinal tubules that can harbor bacteria, and the concept of a single uniform canal opening at the apex is anything but accurate. (8,9) Many teeth will have multiple portals of exit that may or may not be present in the apical third of the root. (Figure 1) As a result, the clinician must assume the apical canal anatomy in every tooth is highly variable in size, shape, and number (10,11,12) and there are no “easy ones.”
maxillary central incisor with a necrotic pulp. A prominent lateral canal can be seen,
but there is no way to know if multiple microscopic branches are present at any level
of the root canal system.
2. The perception of ease may not be accurate when considering anatomy.
Most endodontists will treat the standard four-canal molar in approximately one hour, and I am no different. Obviously some clinicians are more efficient than others and this, along with anatomy, will influence treatment times and outcomes. With this in mind, logic dictates that a premolar should be treated in significantly less time due to increased access with less canal anatomy. However, a significant subset of premolar teeth will require as much or more time to complete than the standard molar root canal due to anatomical complexity. Let’s look at the “easy” teeth in more detail.
ALSO BY DR. LANDWEHR |Electronic determination of working length: more accurate than radiographs?
Maxillary incisors
As an endodontist who sees patients on a referral basis, treating a central incisor is a relatively rare occasion unless the etiology is traumatic in origin. In these cases, the patient is usually younger, and this poses its own challenges with large canals and incompletely developed root ends. If the patient has a history of trauma at a young age, it is not uncommon for pulp canal obliteration to occur, which results in a complete closing of the root canal space and significant difficulty in locating the canal. In spite of age or etiology, there is a shelf of dentin on the lingual just below the cemento-enamel junction (CEJ) that needs to be removed during access or the lingual canal wall will not be cleaned.
Lateral incisors can be relatively long given the overall size of the canal and a curve at the apex is often multiplanar. (13,14)The apex may curve to both the distal and lingual, making it difficult to clean initially or impossible to retreat if the root canal is not successful. (5) As with central incisors, there is a prominent dentin shelf on the lingual at the level of the CEJ, but in contrast to centrals there can be more angulation between the crown and root, resulting in increased difficulty cleaning the lingual wall.
Maxillary canine teeth don't tend to have as much curve at the apex as lateral incisors, but they are very long and can also be large in the buccal-lingual dimension, making it difficult to disrupt and remove biofilm from each of the canal walls. Again, a prominent shelf of dentin is present on the lingual aspect at the CEJ that needs to be removed for straight-line access and the ability to remove biofilm from the lingual wall.
ALSO BY DR. LANDWEHR |Endodontic case study: referred pain leads to diagnostic uncertainty
Mandibular incisors
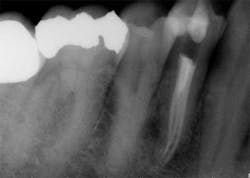
These are my least favorite teeth to treat. Most are heavily restored and the mesial-distal dimension is very small, resulting in no margin for error when locating the pulp chamber. Additionally, there can be significant inclination between the crown and root, and many will have two canals or branching at some level of the canal. (12,15) This lingual inclination of the root results in difficulty obtaining straight-line access into the buccal canal and makes locating the lingual canal almost impossible in some cases, especially if the lingual shelf of dentin is prominent. (Figure 2) Straight-line access into some lingual canals would need to be established through the mid-facial, and this is not a reasonable option for teeth restored with full-coverage crowns. (16)
have two canals. The second canal is lingual
to the main canal, and it is not uncommon for
the two canals to join at the apex. Tooth
No. 24 has a necrotic pulp and based on
the anatomy of teeth Nos. 23 and 26, a
second canal in tooth No. 24 should be expected.
Maxillary premolars
While mandibular incisors are my least favorite teeth to treat, the premolar teeth also provide significant reason for concern as they have highly variable anatomy. The maxillary first and second premolars will have one, two, or three roots and canals. (Figure 3) Maxillary premolar teeth have the smallest mean apical dimension at the apex (11) and the most variable anatomy, with exception of third molars. (12,17) The roots are often very thin, and a bulbous clinical crown may have significant taper to a thin root in the mesial-distal dimension that is broad in the facial-lingual dimension. It is not uncommon to see mesial-distal fractures in maxillary first or second premolars. Maxillary second premolars may have more curvature in the apical portion of the root when the sinus is close to the root ends. (Figure 4)
following root canal treatment in teeth Nos. 4 and 5. An angled
radiograph indicated a high probability for an untreated canal in
tooth No. 4 and as a result, this tooth was retreated.
increased concern about the anatomy in tooth No. 5. This tooth
was subsequently retreated due to persistent symptoms.
were present in both Nos. 4 and 5 following the initial root
canal treatment.
Mandibular premolars
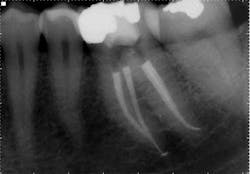
Mandibular premolars can be very difficult to treat and are associated with a high rate of post-treatment disease that is most likely due to anatomic variability. (11) This anatomical variability in mandibular premolars is similar to that of maxillary premolars and is a possible reason why root canal treatment may fail in premolar teeth in general. Similar to maxillary premolars, the clinical crowns taper to a thin root at the CEJ, resulting in very little or no margin for error when accessing the pulp chamber. It is not uncommon to have more than one canal in these teeth. Several studies indicate a second canal is present in more than 25% of mandibular first premolars. (12,15)Often when two canals are present, the second canal is displaced to the lingual and can be very difficult to locate. (Figure 5) Many mandibular first premolars have significant lingual inclination of the root, making the second canal almost impossible to locate because the lingual canal often branches off the main canal at or near a 90-degreeangle. If a single canal is present, it tends to be broad in the buccal-lingual direction, and this makes it difficult to remove biofilm from all root surfaces. Mandibular second premolars also have a high degree of anatomic variability, but not to the same degree as mandibular first premolars. The reported incidence of multiple canals in mandibular second premolars ranges from 1.2% to 29%. (12,18)As with first premolars, many mandibular second premolars have some lingual inclination of the root and a broad buccal-lingual canal dimension results in difficulty contacting all surfaces of the canal with any instrumentation technique.
with conventional radiography, and this branching could be better
visualized with CBCT.
3. Molar teeth have more predictable canal anatomy.
Although there are exceptions to every rule and the potential for anatomic variability has to be considered in every tooth, for the most part molar teeth have consistent root canal anatomies. (12,15) There are well-documented cases of five and six or more canals in molar teeth, but these rare case reports are the exception more than the rule. (19,20) There has been increased awareness about the presence of a mid-mesial canal in mandibular molars over the last several years, and the use of cone beam computerized tomography has increased both our awareness and ability to locate this “extra” canal. (Figure 6) I consider all teeth that I treat to have one more canal than is expected, and so I am never surprised by what I find. If I access a mandibular molar with the expectation that four canals exist (and there could be a fifth or sixth), then the unexpected surprise occurs when only three canals are present. The vast majority of mandibular molars that I treat have four canals: two well-defined mesial canals that may or may not join in the apical one-third of the root and either two distinct canals or a dumbbell shape in the distal root. Because of the broad buccal-lingual dimension of the distal root, I almost always treat this root canal system as though it were two canals.
canal. Although molar teeth can and often do have variable
anatomy, most mandibular molars are going to have at least
three, and more commonly four canals.
in mandibular molars.
No tooth gets more attention than the maxillary first molar because of the MB2 canal or what some clinicians refer to as the mesial-lingual canal. To be most accurate, I refer to this canal as the mesial lingual because in many teeth it has no relationship to the mesial-buccal canal. Without question, the most common questions I get about root canal anatomy relate to this specific canal space. How often is it there? How often can it be located? Where is it located? Does it join the mesial-buccal canal?
These are important questions that deserve more attention, because this canal can be difficult to locate and difficult to negotiate to the apex. By my way of thinking and practicing, every maxillary molar tooth has at least four canals. (Figure 7) This mindset helps me stay focused and determined to locate all of the canals. Some mesial-lingual canals are located at the level of the pulp chamber directly lingual to the mesial-buccal canal, and these canals are going to be more easily located than the ones that are 1 mm or 2 mm apical to the pulpal floor and significantly more mesial than the mesial buccal. Bottom line: The mesial-lingual canal orifice is variable in its lingual extent and in both the mesial-distal and coronal-apical position, but it is present with such a high frequency that a thorough exploration of the area, aided by enhanced magnification and illumination, should yield positive results in 90% of maxillary first molars and a slightly lower percentage in maxillary second molars. (20) In my experience, the closer the two canals are at the chamber level, the more likely they are to join. Again, there are exceptions to this and every rule, but these exceptions comprise a very small percentage of cases.
mesial buccal root of maxillary first molars. This tooth initially
had three distinct canals in the mesial buccal root. Following
final shaping, two canals joined at various levels, but the third
canal had no connection.
buccal canals. The two canals were very close in the chamber,
but branched in the apical portion of the root to exit via
distinct openings.
of the maxillary molar: four canals total with the two canals in
the mesial buccal root joining to exit a common foramen.
Molar teeth, both maxillary and mandibular, present challenges to the clinician because multiple canals are present and access can be limited, making visualization and rubber dam placement more challenging compared to other groups of teeth. However, the anatomy is often less variable and more easily located in molar teeth and a greater amount of tooth structure is available, thereby increasing the margin for error. Access and line of sight may be more straightforward in premolar and anterior teeth, but anatomical variability is common. In many instances, the anterior and premolar roots have a small mesial-distal dimension and making an ideal access opening to locate canals and preserve tooth and root structure for restoration becomes difficult. When the frequent branching occurs in anterior and premolar teeth, it will usually happen well below the pulpal floor at the mid-root level of the canal and this makes locating and cleaning many of these spaces very difficult and nearly impossible. Because the number of root canals can be variable and the shape, size, amount, and location of the microanatomy is unpredictable in all teeth, I think it is fair to say that no root canal treatments should be considered “easy.”
This article first appeared in the newsletter, DE's Breakthrough Clinical with Stacey Simmons, DDS. Subscribe here.
ALSO BY DR. LANDWEHR |There is more than one way to skin a cat: Deciding which endodontic file will achieve the best clinical outcome
References
1. Kakehashi S, Stanley HR, Fitzgerald RT: The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surg. 1965;20:340.
2. Wada M, Takase T, Nakanuma K, Arisue K, Nagahama F, Yamazaki M. Clinical study of refractory apical periodontitis treated by apicoectomy. 1. Root canal morphology of resected apex. Int Endod J. 1998;31:53.
3. Kuttler Y. Microscopic investigation of root apexes. J Am Dent Assoc. 1955;50:544.
4. Simon JHS. The apex: how critical is it? Gen Dent. 1994;42:330.
5. Mizutani T, Ohno N, Nakamura H. Anatomical study of the root apex in the maxillary anterior teeth. J Endod. 1992;18(7):344.
6. Peters OA, Laib A, Gohring TN, Barbakow F. Changes in root canal geometry after preparation assessed by high-resolution computed tomography. J Endod. 2001;27(1):1.
7. Mickel AK, Chogle S, Liddle J, Huffacker K, Jones JJ. The role of apical size determination and enlargement in the reduction of intracanal bacteria. J Endod. 2007;33:21.
8. Mjör IA, Nordahl I. The density and branching of dentinal tubules in human teeth. Arch Oral Biol. 1996;41:401.
9. Mjör IA, Smith MR, Ferrari M, Mannocei F. The structure of dentin in the apical region of human teeth. Int Endod J. 2001;34(5):346.
10. Caliskan MK, Pehlivan Y, Sepetcioglu F, Turkun M, Tuncer SS. Root canal morphology of human permanent teeth in a Turkish population. J Endod. 1995;21(4):200.
11. Morfis A, Sylaras SN, Georgopoulou M, Kernani M, Prountzos F. Study of the apices of human permanent teeth with the use of a scanning electron microscope. Oral Surg Oral Med Oral Pathol. 1994;77(2):172.
12. Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58:589.
13. Chohayeb AA. Dilaceration of permanent upper lateral incisors: Frequency, direction, and endodontic treatment implications. Oral Surg Oral Med Oral Pathol. 1983;55(5):519.
14. Park PS, Kim KD, Perinpanayagam H, Lee JK, Chang SW, Chung SH, Kaufman B, Zhu Q, Safavi KE, Kum KY. Three-dimensional analysis of root canal curvature and direction of maxillary lateral incisors by using cone-beam computed tomography. J Endod. 2013;39:1129.
15. Pineda F, Kuttler Y. Mesiodistal and buccolingual roentgenographic investigation of 7275 root canals. Oral Surg Oral Med Oral Pathol. 1972;33:101.
16. LaTurno SAL, Zillich RM. Straight-line endodontic access to anterior teeth. Oral Surg 1985;59:418.
17. Carnes EJ, Skidmore AE. Configurations and deviation of root canals of maxillary first premolars. Oral Surg Oral Med Oral Pathol. 1973;36(6):880.
18. Sert S, Bayirli GS. Evaluation of the root canal configurations of the mandibular and maxillary permanent teeth by gender in the Turkish population. J Endod. 2004;30(6):391.
19. Beatty RG, Krell K. Mandibular molars with five canals: report of two cases. J Am Dent Assoc. 1987;114(6):802.
20. Beatty RG. A five-canal maxillary first molar. J Endod. 1984;10(4):156.
21. Gilles J, Reader A. An SEM investigation of the mesiolingual canal in human maxillary first and second molars. Oral Surg Oral Med Oral Pathol. 1990;70(5):638.