Eye safety in dentistry
Abstract
The objective of this article is to express an experimental, work-supported opinion of its authors regarding the inadequacy of the current dental mask and eyewear combination for protecting dental providers. The various types and sources of dental practice eye occupational hazards and the possible entry routes of dental debris toward the practitioner’s eyes are discussed. Experimental work investigating the shortcomings of the current dental mask and eyewear combination for protecting the dental provider’s eyes are presented.
Authors’ note: The opinions expressed in this article are solely those of the authors and do not represent opinions, positions, or recommendations—express or implied—made by The University of Massachusetts Lowell or by Tufts University. These opinions are based on Dr. Peter Arsenault’s extensive experience as a practicing dentist and as a professor of operative dentistry and Dr. Amad Tayebi’s extensive experience in the design and manufacturing of NIOSH-approved respiratory protection devices. In the interest of transparency, the authors hereby disclose that they are co-inventors of a patent covering a mask with debris deflector.
Types and sources of dental practice eye occupational hazards
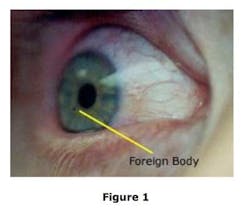
By their nature, dental procedures involving drilling at very high speeds (180,000 rpm to 500,000 rpm) generate debris traveling at speeds of up to 50 mph. Such debris includes pieces of amalgam, tooth enamel, calculus, pumice, and broken dental burs along with blood-borne pathogens. In the absence of protective means, such debris may find its way to the eyes of the dental practitioner or dental assistant (Figure 1; Source: Google Photos).
ADDITIONAL READING | Jenn’s vision: A true lesson in best practices
Normally, dentists, hygienists, and dental assistants wear masks and protective eyewear (glasses: prescription, nonprescription, and loupes) while performing dental procedures. Dental masks are available in a variety of designs and profiles, including pleated, molded cup, duckbill, and foldable styles. The most commonly used type is the pleated style. All dental mask styles provide protection of covered facial areas—primarily the nose, mouth, and portions of the cheeks—against splash.
Pleated dental masks are most preferred by dental practitioners since they are easy to wear and have low resistance to breathing.
Masks fitted with a full-face transparent shield are particularly desirable because a dental procedure can potentially generate the splashing of blood-borne pathogens and various debris. Masks with a full-face shield worn with appropriate eyewear underneath provide the most effective facial and eye protection against such safety hazards.
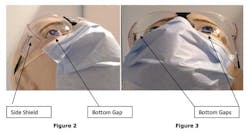
Referring to Figures 2 and 3, there are three possible routes dental debris may follow in order to reach the eye of a practitioner not wearing a full-face shield mask, namely:
- Frontal Entry Routeby debris traveling perpendicular to the practitioner’s face. Glasses provide the necessary protection against such debris. They are required by OSHA Standard 1910.133(a) (1) and must meet ANSI Standard (Z87.1). Accordingly, fewer eye injuries are caused by such debris.
- Sideways (right to left or left to right) Entry Routesby debris traveling tangential to the face. Side shields provide effective protection against such debris and are specifically required by OSHA Standard 1910.133(a) (2).
- Bottom Gaps Entry Routes by debris traveling vertically and tangential to the face. Such debris may reach a practitioner’s eye through the open gaps (bottom gaps) between the lower rims of the lenses of the protective eyewear and the upper edge of the mask worn by the practitioner.
As discussed above, since Front Entry Route and Sideways Entry Routes are effectively blocked by the use of OSHA-required protective eyewear (OSHA Standard 1910.133(a)(1)) and side shields (OSHA Standard 1910.133(a)(2)), the Bottom Gaps Entry Routes are the most frequent, yet unaddressed, routes of eye-injury-causing debris.
Experimental work
A series of spray studies were conducted to evaluate the efficiency and safety of the current, typical personal protective equipment used in the dental setting.
The objective of the experimental spray studies were to evaluate the entry routes associated with the noted bottom gaps (the spaces between the wearer’s cheek or top edge of the worn mask and the bottom rim of the worn eyewear (see Figures 2 and 3) when a red-dyed spray was directed at the simulated practitioner’s face from different angles.
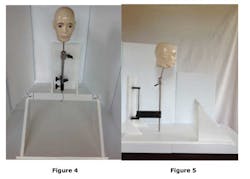
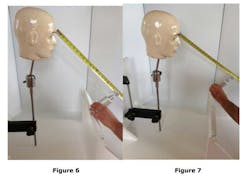
Experimental set-up and proceduresAn apparatus was constructed to simulate the angles where a dentist or dental hygienist would most likely be relative to the patient and the dental handpiece used during typical dental procedures. (See Figures 4, 5, 6, and 7) Because of the nature of the study, a medium-size mannequin head was used as the subject as opposed to a “live” subject.
A spray bottle containing water-base red dye was used for spraying the dye solution at the mannequin head from the six o'clock (middle position), four o’clock, and eight o'clock positions (left and right positions) to simulate the average, typical angles that would be consistent with the dentist/patient operating positions and angles.
The first spray study consisted of the mannequin head wearing OSHA-compliant safety glasses with side shields along with a standard, flat ear loop mask (See Figure 8). The second spray study consisted of the mannequin head wearing a mask with a full-face shield without eyewear under the full-face shield/mask combination (See Figure 9).
With the mannequin head in both studies mounted at the exact same position and angles with relation to the nozzle of the spray bottle, the nozzle was aimed at the mannequin head from the above-mentioned positions. Two complete spray shots from the spray bottle were generated from each of the three positions to evaluate possible entry routes for debris projectiles and associated procedural fluids. This was repeated for both mask set-ups.
V conclusion, results, and discussion
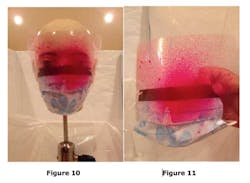
The first spray study was conducted with the mannequin head wearing a mask with full-face shield, (see Figure 9). With the head mounted as outlined (see Figures 4, 5, 6, and 7), two spray shots were directed at the mannequin head from the above-mentioned three positions. The results showed that a mask with a full-face shield provided complete and adequate facial protection from the typical spray and debris paths that a dental provider would encounter during a dental procedure (See Figures 10, 11, and 12). Note that the mannequin's eyes are clear from the spray dye (see Figure 12) indicating that the bottom gaps were adequately blocked while wearing the full-face shield/mask combination during the spray study.
As shown in Figures 13 and 14, it is clear that the spray dye covered the bottom rim of the safety glasses and the top edge of the mask while penetrating through the open bottom gaps and proceeding to the mannequin's eyes by traveling vertically and tangential to the face (See Figures 15, 16, and 17).
These findings demonstrate clearly that there is a major inadequacy and breach of the present dental mask and eyewear combination for protecting the eyes of a dental care provider. Closing the bottom gaps are essential to protect the eyes from dental debris along with blood-borne pathogens that may reach the eyes of the dental provider through such bottom gaps.
Suggested reading 1. Colvin J. Eye injuries and the dentist. Australian Dental Journal. Dec. 1978. 2. Farrier SL, Farrier JN, Gilmour ASM. Eye safety in operative dentistry—a study in general dental practice. British Dental Journal. Feb. 2006. 3.Ajayi YO, Ajayi EO. Prevalence of ocular injury and the use of protective eye wear among the dental personnel in a teaching hospital. Nig Q J Hospital Med. Apr.-Jun. 2008. 4. Roberts-Harry TJ, Cass AE, Jagger JD. Ocular injury and infection in dental practice—a survey and a review of the literature. British Dental Journal. Jan. 5, 1991. 5. Sims APT. Roberts-Harry TJ. Roberts-Harry DP. The incidence and prevention of ocular injuries in orthodontic practice. British Journal of Orthodontics. Nov. 1993. 6. Hartley JL. Eye and facial injuries resulting from dental procedures. Dental Clinics of North America. July 1978;22(3). 7. Wesson MD, John B. Thornton JB. Eye protection and ocular complications in the dental office. General Dentistry. Jan.-Feb. 1989. 8. Khalid A. Wazzan A, Almas K, et al. Prevalence of ocular injuries, conjunctivitis and use of eye protection among dental personnel in Riyadh, Saudi Arabia. International Dental Journal. 2001; 51(2). 9. Cooley RL, Cottingham AJ, Abrams H, et al. Ocular injuries sustained in the dental office: methods of detection, treatment, and prevention. JADA. Dec. 1978;97. 10. Needleman MS, McLaughlin DK, Orner G, et al. Eye hazards among a dental school population. Journal of Dental Education. Sept. 1977; 41(9). 11. Miller J. Eye injuries: a hazard in the dental office. Oklahoma Dental Association. Winter 1985;75(3). 12. Stokes AN, Burton JF, Beale R. Eye protection in dental practice. New Zealand Dental Journal. 1990;86:14-15. 13. Kelsch NB. Protecting eyes: What? RDH Magazine. August 2012. 14. Jorgensen G. Protecting your eyes. Dentistry IQ. May 2014.