Avoiding common pitfalls in endodontic diagnosis
Endodontic therapy involves multiple steps in order to achieve success. Making the correct diagnosis is imperative in order to set the stage for a successful outcome. The purpose of this article is to identify the common pitfalls and review the correct steps in the endodontic exam and diagnosis.
Establish a routine
Establishing a reproducible routine is a key component to diagnostic success. The patient will often present with diagnostic challenges that can be confusing. An organized and consistent approach is imperative. It is natural to empathize with a patient and try to relieve the pain quickly. Resist the urge to rush to make a diagnosis before a complete exam.
What is the chief complaint?
Identify the chief complaint. Remember to stop talking and listen. Ask the patient the following questions:
- Are you having pain?
- Can you describe the pain?
- Is the pain spontaneous, throbbing, short and sharp, or lingering?
- Is the pain brought on by hot cold or pressure?
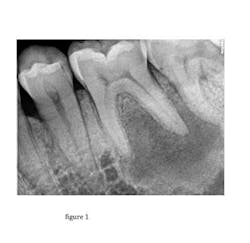
Radiographic exam
Take quality radiographs that are angulated correctly. Often two or more angles are necessary. Look for evidence of faulty restorations, caries, or changes in the PDL or periradicular radiolucent areas. This is also an opportunity to begin to appreciate the anatomy and potential complications that may arise in treatment. After radiographs are obtained, the answers to the previous questions can begin to be correlated with radiographic findings. A common error is to make a diagnosis before completing all phases of the exam.
The clinical exam
The clinical exam should always be preceded by a complete and thorough review of the medical history. While it is beyond the scope of this article, it should be noted that a nonodontogenic source for symptoms mimicking endodontic pain is possible.
The clinical exam consists of both an extraoral and intraoral exam.
Extraoral exam
The key elements of the extraoral exam are to palpate the TMJ and associated muscles. Myofacial pain is often confused with endodontic pain.Intraoral exam
Percussion — Remember that pain to percussion is only a sign of inflammation in the periradicular tissues. Percussion sensitivity can be associated with many different etiologies. This includes pulpal and or periradiclular disease, traumatic occlusion, TMD and nonodontogenic causes. While percussion is a key component, this test alone does not determine the endodontic diagnosis. (Figure 2)
Palpation — Palpate in the area of the root apices. This is the most common area for pain with palpation to manifest itself when it is associated with a diseased pulp. (Figure 3)
Thermal testing — Thermal testing is a key component in endodontic diagnosis. The most simple and common thermal test is the cold test. A useful tool is refrigerant spray, which is easily applied to a cotton pellet. The cold pellet is then placed on the tooth, approximating the location of the pulp chamber. If a crown is present, place the cold closer to the crown margin.
Refrigerant spray — First establish a baseline with thermal tests. Before testing the suspected area, establish a normal in a different quadrant. (Figure 4)
• Mild to moderate, minimal lingering — normal
• Moderate, lingering — abnormal
The following guidelines can be used to interpret the cold test results:
Severe — abnormal
No response — abnormal or normal dependent on control test
When a patient complains of pain with heat, there are some simple ways to complete a hot test. Asking the patient to take a sip of hot water will reproduce the discomfort. Once the pain is present, apply cold to the suspected tooth. The pain will immediately subside once the offending tooth is cooled. This test may take multiple attempts to identify the source of pain, but similar to the cold test, it can be dramatic in its usefulness in identifying the source of pain.
Periodontal exam
Examine the area for swelling, sinus tracts, and probing depths. In the case of a vertical fracture, a narrow periodontal pocket may be located. (Figure 5)
After the complete exam, the information can be organized in a thoughtful and logical manner. This will lead to making a consistent and accurate endodontic diagnosis.
Editor’s note: This article appeared in Chairside Daily newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles at this link and subscribe here.
Michael Zuroff, DDS, graduated from University of Detroit School of Dentistry. He completed one year of general practice residency at Sinai Hospital in Detroit. Dr. Zuroff attended New York University for his postgraduate training in endodontics, was awarded for his postgrad research at the American Association of Endodontics annual session in 1995, and has been published in the Journal of Endodontics. Dr. Zuroff is also a graduate and fellow at the Misch Implant Institute and has a special interest in bone grafting and implant surgery. He has lectured extensively on endodontics as well as implants. He and his wife Cheryl have three children.
Recommended