The dental professional's role in HIV education: It's an ethical responsibility
By Diana Macri, RDH
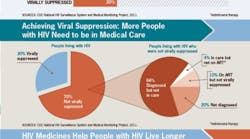
In its most recent issue of Vital Signs Monthly, the CDC reported that 86% of HIV-positive Americans are diagnosed but only 37% are prescribed antiretroviral medicines. This means a very high number of Americans are not receiving the antiretroviral therapy necessary to suppress the disease. Viral suppression means having very low levels of HIV in the body, even though the virus is still there. An HIV-positive person taking ART can expect to live a normal lifespan, comparable in every way to an individual who does not have HIV and have a very low risk for transmitting HIV to others.
Although HIV incidence and HIV-related deaths have seen declines of approximately 30% globally since 2005, an estimated 1.5 million fathers, mothers, sons, and daughters died from AIDS in 2013. The prevalence of viral suppression was significantly lower among persons aged 18–24 years (13%), 25–34 years (23%), and 35–44 years (27%) compared with those aged 65 years or older (37%). Approximately 66% of persons who did not have a suppressed viral load were diagnosed with HIV but not engaged in HIV medical care.
Anyone who is diagnosed as HIV-positive should receive medical care, and be offered ART as soon as possible. Early ART reduces the likelihood of sexual transmission of HIV by 96%. The crucial step, then, is get these patients connected to medical care systems and continually provide support and resources to keep them committed to taking the medication. This will increase both the quality and length of their lives and significantly reduce the chances of them transmitting the virus to others.
In a recent study that explored the reasons for non-adherence to the ART regimen, researchers list lifestyle differences, decreased awareness of mortality (and thus motivation to care for one’s health), and alcohol use. Black and Hispanic race/ethnicity, female gender, receipt of public assistance, feeling depressed, and number of daily ARV doses were also independently associated with poorer adherence for at least two of the three measures of nonadherence.
Interestingly, the study also cited distrust of physicians or HIV conspiracy beliefs (for example, the belief that HIV was created by the U.S. government to perpetrate genocide against blacks) as reasons for nonadherence, which, to me, supports the need for mental health therapies as well.
Achieving viral suppression requires the use of ART regimens with at least two, and preferably three, active drugs from two or more drug classes. When initial suppression is not achieved or is lost, rapidly changing to a new regimen with at least two active drugs is required. According to the U. S. Department of Health of Human Services “Achieving treatment goals requires a balance of sometimes competing considerations. Regimens should be tailored for the individual patient to enhance adherence and thus improve long-term treatment success. Individual regimen choice is based on such considerations as expected side effects, convenience, comorbidities, interactions with concomitant medications, and results of pretreatment genotypic drug-resistance testing.”
The CDC recommends that doctors, nurses, and health care systems:
- Test patients for HIV as a regular part of medical care.
- Counsel patients who do not have HIV on how to prevent it.
- Make sure people living with HIV are prescribed and take HIV medicines, stay in care and get supportive services such as nutrition, housing, or mental health services.
- Work with health departments to get and keep people in HIV medical care.
Last year, I was lucky enough to participate in a program coordinated by the NY/NJ AETC (New York/New Jersey AIDS Education and Training Center) which conducts targeted, multi-disciplinary education and training programs for health-care providers treating persons living with HIV/AIDS. As part of the oral health preceptorship program I spent two days shadowing the doctors at North Shore-LIJ as they provided care to patients with HIV/AIDS.
The doctor who I was assigned to work with, Dr. Joseph McGowan, spent a great deal of time educating me about the science behind the therapies, the specific medications and their effects, the funding challenges and, most importantly, the personal frustrations health-care providers face as they struggle to get these patients to commit to taking the therapies. I am very grateful to him and the staff at NY/NJ AETC for teaching me so much. Because of this experience I have a better understanding of how important it is that we all keep up the education efforts that have proven to be so successful in preventing infection.
The CDC Vital Signs monthly report was launched in 2010. It is released the first Tuesday of every month and covers various topics including colorectal and breast cancer screening, obesity, alcohol and tobacco use, HIV testing, motor vehicle safety, cardiovascular disease, teen pregnancy and health-care-associated infections, foodborne disease and more. You can sign up to get Vital Signs each month at http://www.cdc.gov/vitalsigns/hiv-aids-medical-care/index.html. Most of the materials are available in English and Spanish.
Dental hygienists are oral health specialists, but are also health-care providers. It is our ethical responsibility to be aware of the many health-care issues our patients may face and to share that information with our patients so they may lead healthier, more productive lives. It has been proposed by some that oral health professionals should begin HIV testing as part of a dental care appointment utilizing a rapid, noninvasive test done on oral fluids. Results are available within 20 minutes, and it has high sensitivity and specificity comparable to blood testing.