Orthodontic options for the ectopic eruption of a maxillary first molar
The transitional dentition period often presents with a multitude of challenges for the practitioner to manage. Ectopic eruption is one of those problems that if diagnosed and treated early, the prevention of malocclusion issues can easily be prevented.
ALSO BY DR. STACEY SIMMONS |Consideration of nonsurgical compromises in Class II orthodontic cases
Ectopic eruption is a disturbance in which the tooth does not follow its usual course. (1) Nikiforuk furthermore defined ectopic eruption as “a condition in which the permanent teeth, because of deficiency of growth in the jaw or segment of jaw, assume a path of eruption that intercepts a primary tooth, causes its premature loss, and produces a consequent malposition of the permanent tooth. (2) Failure to treat ectopic eruption can result in loss of arch length, inadequate space for the succeeding premolar, and malocclusion. (1) This report will focus on the ectopic eruption of the first molar.
ALSO BY DR. STACEY SIMMONS | Impacted canines and orthodontic treatment
The causes for ectopic eruption, as reported by Chapman, (3) include:
- Early eruption of the maxillary first permanent molars
- Lack of forward movement of all primary teeth
- Deviant paths of eruption of the permanent molar
- Small arch
When the balance of timing and rate of growth are disrupted due to environmental interferences or congenital factors (i.e., rate of jaw growth, rate of eruption of first molar, and/or sizes of the teeth), an abnormal situation develops. (1)
The incidence of ectopic eruption of first molars was reported by Young in 1957. A case study of 1,619 boys and girls revealed a 3% incidence of ectopic eruption and was most often observed in the maxilla. (4) This anomaly was observed 19 times in girls and 33 times in boys. (4) Untreated correction was also noted to be higher in girls. (4)
There are two classifications of ectopic eruption — reversible and irreversible/locked. Reversible is when a molar will erupt into its essential normal position without corrective treatment. (4) Irreversible/locked is when the molar remains in location until it is acted upon (or unlocked) or the primary second molar is exfoliated. (4) In a study conducted by Young, 66% of ectopically erupting molars erupted into their normal position without corrective treatment. (5)
Examination of bitewing and periapical radiographs is how ectopic eruptions are most commonly diagnosed. When an impacted first permanent molar has not erupted or is only partially erupted, the treatment of choice is watchful waiting because more than half of the teeth will eventually erupt into normal position (66%). (4, 5) A report by Bjerklin and Kurol indicates that ectopic permanent molars of the reversible type had freed themselves by the time the patient reached 7 years of age, but that only a few molars of the locked or irreversible type had freed themselves by this age. (5,6) This study furthermore indicated that diagnosis of a reversible or irreversible status can be determined between the ages of 7 and 8 years old. (6)
There are several treatment and management options for ectopically erupting first molars. These include interproximal wedging and distal tipping, both of which cause incremental distocclusal movement via various techniques. (1, 5)
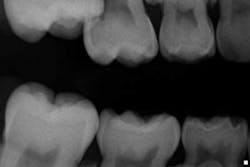
Case report A healthy 7-year-old female presents for a routine examination and cleaning (she had not been seen for two years). Crowding was noted primarily in the mandibular arch; the maxilla had a high palate. A significant amount of plaque/debris was noted in the upper right area between partially erupted No. 3 and tooth A. A bitewing radiograph on the right side barely revealed an ectopic eruption of tooth No. 3. (Fig. 1)Fig. 1Periapical and panoramic radiographs were taken and exposed a 50% resorption of the distal root and pulp chamber of tooth A. (Figs. 2 and 3)
Fig. 2
Fig. 3Tooth A was not mobile nor was there any pain or discomfort to the area (despite the moderate amounts of plaque and debris). A referral was made to an orthodontist.
Fig. 4
The following was discussed post-consultation with the orthodontist:
- The mesial drifting of No. 3 was severe enough that it was diagnosed as an irreversible case of ectopic eruption.
- The eruption potential of tooth No. 4 was impeded.
- Leaving the status quo would create a concern for bacterial entrapment and potential abscess; therefore, it was agreed upon that tooth A needed to be removed.
- Upon removal of tooth A, these options were presented to the parents:
- If agreeable to Phase I orthodontics, a palatal expander would be placed and #No. 3 would be distalized so No. 4 would be able to erupt into the arch. This would not necessarily eliminate phase II orthodontics in the future, but the potential for fewer complications would be in the patient’s favor.
- If not agreeable to Phase I, then a space maintainer would be utilized to hold the space as much as possible until a definitive treatment plan could be devised that would be agreeable to the parents. A Nance appliance would suffice to hold the space.
At the time of this write-up, the patient was scheduled to begin Phase I treatment with subsequent extraction of tooth A. It is anticipated that the results will be favorable.
Acknowledgement: The author would like to recognize Dr. Padraig Dennehy for his insight to the write-up and case report of this article. He can be reached at [email protected] and www.dennehyorthodontics.com.
References
1. Yassen SM, Naik S, Uloppi KS. Ectopic eruption: A review and case report. Contemporary Clinical Dentistry. Jan.-Mar. 2011;2(1):3-7.
2. Nikiforuk G. Ectopic eruption: Discussion and clinical report. J Ont Dent Association. 1948;25:243-246.
3. Chapman H. First upper permanent molar partially impacted against second deciduous molar. Int J ortho Oral Surgery and Radiology. 1923;9:339-345.
4. Young DH. Ectopic eruption of the first permanent molar. Journal Dentistry Child. 1957;24:153-162.
5. McDonald R, Avery D, Dean J. Dentistry for the Child and Adolescent. 659-660. 8th Edition. 2004. Mosby.
6. Bjerklin K, Kurol J. Ectopic eruption of the maxillary first permanent molar: Etiologic factors. American Journal of Orthodontics. 1983;84:147-155.