The impact of patient and payer mix on dental program sustainability
In his first two articles, Dr. Mark Doherty described what a safety net dental program is: The dental care safety net is where people go:
• When they don't have a regular dentist
• Because they know their Medicaid card will be accepted
• Because they won't be turned away when they are in pain and can't afford care
• Because the clinic is close to home and linked to their other health care providers
In this article, Dr. Doherty describes the importance of patient and payer mix on dental program sustainability.
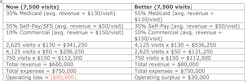
In safety net dental programs, payer mix has a huge impact on financial sustainability, and can be a significant challenge to manage. To understand the impact payer mix is having on the dental program, dental leadership first needs to determine the average revenue per visit for each payer type (e.g., Medicaid, Medicaid Managed Care, commercial, and self-pay/sliding fee scale patients). This is an easy process (net revenue per payer type divided by number of visits per payer type).
With average revenue per visit per payer type in hand, leadership can identify a payer mix that ensures financial sustainability while preserving access for all patients. The following table provides an example of the impact of payer mix on sustainability.
The most effective way to tweak the payer mix is to designate priority populations and develop action steps to recruit more of these patients into the dental program. Pregnant women and children are more likely to have Medicaid insurance. In addition, there are good clinical reasons for designating women and children as priority patients. For example, prevention and elimination of dental disease in pregnant women decreases the likelihood of transmission to infants, and the same focus in children improves the chances of them growing into disease-free adults.
In health centers with medical services, integration of medical and dental care ensures a pathway for children and pregnant women from medical to dental. Standalone safety net dental programs will need to establish referral relationships with external agencies that serve children and pregnant women to ensure more priority patients have access to dental care.
Since capacity is finite, increasing the number of Medicaid patients in the practice comes at the expense of access for uninsured patients. The goal is to preserve as much access as possible for uninsured patients while maintaining financial sustainability. Operating the dental program in the black lays the groundwork for future expansion, which eventually increases access for all patients.With average revenue per visit per payer type in hand, leadership can identify a payer mix that ensures financial sustainability while preserving access for all patients. The following table provides an example of the impact of payer mix on sustainability.
READ DR. DOHERTY'S FIRST TWO ARTICLES:How to create and manage a successful safety net dental program
Using the fee schedule to create sustainability and affordability in the dental practice
Mark Doherty, DMD, is the Director of Safety Net Solutions at the DentaQuest Institute.