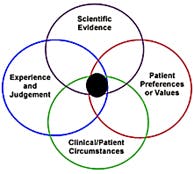
Presentation topics at the Conference included: Why is Science-Based Medicine Important?; Barriers to Implementing EBD; Barriers to Implementing EBD; Learn How to Critically Appraise a Systematic Review; Strategies for Teaching EBD; Implementing EBD Into Schools; Implementing Science in Policy; Quality Measures and the Dental Quality Alliance; Patient-Centered Outcomes and Comparative Effectiveness Research; and many other topics.MPG: In your opinion, why is EBD important?Dr. Gillette: I believe EBD is important to keep practitioners current with changes in treatments and products. It is similar to Continuing Education (CE) but more structured. It involves asking a focused question, doing a literature search to find manuscripts to answer questions posed by the clinician and evaluating the evidence for scientific rigor and bias, consistency of results, and volume of evidence. It also helps to resolve issues around conflicting messages, such as the efficacy of non-fluoride caries preventing agents, which can be confusing. As an example, in 2011 the ADA developed a clinical guideline on that topic which included a systematic review. Grades were given on the strength of the evidence, and a simple chairside guide was created for ease of use by the practicing dentist or dental hygienist. (1,2) It is like peeling off layers of an onion, you peel off as much information as you need or have time for. If you’re super busy you might just use the chairside guide to assist in your clinical decision-making, but if you want to know more you can go to the full guideline. Also, I believe the Commission on Dental Accreditation (CODA) provides some guidance to dental schools in the Accreditation Standards for Dental Education Programs.(3,4) “These competencies must be reflective of an evidence-based definition of general dentistry.”(5) Evidence-based care is defined in the document, and mentioned in several places throughout the Standards. * Editor’s note: “Evidence-based treatment strategies” in mentioned in the Accreditation Standards for Dental Hygiene Education Programs, on page 22, where evidence of compliance of “2-17 Graduates must be competent in providing the dental hygiene process of care …” “d) provision of patient-centered treatment and evidence-based care in a manner minimizing risk and optimizing oral health” can be demonstrated with evidence-based treatment strategies.(6) Evidence-based practice is also mentioned in 2-25: “Graduates must be competent in the evaluation of current scientific literature.”MPG: Do you think dental hygiene programs should also be teaching EBD, in addition to dental schools?
Montana clinical research dentist and practitioner, Dr. Jane Gillette is a nationally recognized leader in primary oral disease prevention, health disparities and evidence-based dentistry. For more on Dr. Gillette, visit http://www.sproutoralhealth.org/.RELATED | Evidence-based diagnostic standards for temporomandibular disorders
References 1. Rethman MP, Beltrán-Aguilar ED, Billings RJ, Burne RA, et al. Nonfluoride caries-preventive agents: Executive summary of evidence-based clinical recommendations. JADA, 142 (9):1065-1071, 2011. http://jada.ada.org/content/142/9/1065.full.pdf+html. 2. http://ebdlegacy.ada.org/ClinicalRecommendations.aspx. 3. http://www.ada.org/en/coda. 4. http://www.ada.org/~/media/CODA/Files/predoc_2013.ashx. Accreditation Standards for Dental Education Programs. 5. http://www.ada.org/~/media/CODA/Files/predoc_2013.ashx. Accreditation Standards for Dental Education Programs, page 10. 6. Accreditation Standards for Dental Hygiene Education Programs, page 22. http://www.ada.org/~/media/ADA/Education%20and%20Careers/Files/dh.ashx. 7. http://ebdlegacy.ada.org/. 8. http://www.cebd.org/. 9. http://www.amazon.com/Evidence-Based-Decision-Making-Translational-Professionals/dp/0781765331. 10. http://www.dentalcare.com/en-US/dental-education/continuing-education/ce311/ce311.aspx?review=true.Additional Resources 1. Agency for Healthcare Research and Quality: Evidence-Based Decisionmaking. http://www.ahrq.gov/professionals/prevention-chronic-care/decision/.More by Maria Perno Goldie:Crohn's diseaseReport from the 43rd Annual Meeting & Exhibition of the American Association for Dental Research