Endodontic case study: Healing of a large lesion in a lower molar after proper dental instrumentation and irrigation
Clinician: Aneel Belani, DDS
Description of the tooth: Lower molar No. 31 of a 52-year-old female patient
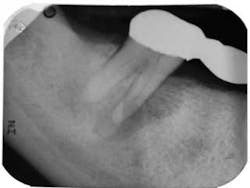
Diagnosis: Pulpal necrosis with chronic periradicular abscess
A 52-year-old female patient presented to our office for consultation on tooth No. 31 with the chief complaint: “My dentist says I need to have my tooth pulled, but I want to see if I can save it.” Medical history was noncontributory. Patient had a bridge placed more than five years ago from Nos. 29 through 31. She had a history of mild discomfort in the area of No. 31, but had not had any serious problems until two months prior when a fistula had developed. She visited her dentist, who took radiographs and deemed tooth No. 31 fractured and nonrestorable. She had been referred to a periodontist for extraction of No. 31 and implant placement in areas of No. 30 and No. 31. Having been to our office for previous endodontic therapy, the patient returned for a second opinion.
RELATED |Periodontal abscess, endodontic abscess, or a combination: How to decipher
Clinical evaluation revealed a draining fistula on the buccal aspect of tooth No. 31. Endodontic testing revealed tooth No. 31 had no response to cold, no pain to percussion, 7-8 mm probing depths on its distal aspect, and pain on palpation. All other teeth in the quadrant tested normal. The diagnosis was pulpal necrosis with chronic periradicular abscess. The patient was advised that the prognosis was guarded, but if she wanted to try to save the tooth, we could try.
RELATED |Considerations in dental treatment planning: Focus on revision of failed endodontic cases
The patient was anesthetized using two carpules of 2% lidocaine for IANB and two carpules of Septocaine for long buccal infiltration. The tooth was isolated with a rubber dam and accessed under a dental operating microscope using long shank round burs and an Endo-Z bur for refining the access to cavity walls. Working length was determined using Root ZX II electronic apex locator. Instrumentation was completed using Xgates, and a combination between Protaper and Vortex Blue files with full-strength sodium hypochlorite irrigation. QMix was placed into the canals after irrigation and agitated with EndoActivator to remove the smear layer and for its antibacterial properties. Calcium hydroxide was placed, and the root canal was temporized with TERM temporary.
On the second appointment, the calcium hydroxide was rinsed out and the canals reinstrumented. QMix was again placed into the canals and agitated with EndoActivator. The canals were filled using warm vertical condensation with System B and Calamus backfill. The patient was given a six-month follow-up appointment and ibuprofen 600 mg for postoperative discomfort. I again stressed to the patient that the prognosis for this tooth was guarded. At the six-month follow-up appointment, the patient had been asymptomatic and there was clear evidence of healing.