Subgingival anomalies and pathologies viewed with the Perioscope
Since its inception more than a decade ago, the Perioscopy System has become a “secret weapon” in non-surgical periodontal therapy among a small group of clinicians called the Early Adopters.
The Perioscopy system consists of a tiny fiberoptic camera less than a milimeter which illuminates and magnifies the subgingival environment up to 48 times. The camera, attached to a dental probe (Perioscopy Explorer) is placed gently below the gum line and a video image is immediately displayed on a chairside monitor, disclosing minute details that previously may have been undetectable such as root fractures, decay, resorption, and of course, calculus.
This small camera allows clinicians to diagnose and or treat simultaneously in the most minimally invasive, non-surgical manner possible and has been found to not only aid in the overall health of the periodontium, but many times the patient appears to regenerate bone post treatment of subgingival debridement.
This series of articles explores various anomalies and pathologies visualized with the Perioscope, which have been found to be contributing factors in localized periodontal breakdown.
Prior to Perioscopy, many of these areas would have required surgical intervention to view. The Perioscopy System provides the most minimally invasive, non-surgical alternative available, with little to no post treatment discomfort or “downtime” for the patient.
Article one delves into the complexities of external root resorption.
Root Resorption:
In their Abstract “Root resorption – diagnosis, classification and treatment choices based on stimulation factors”, Fuss, Tsesis and Lin stated “etiology of different types of root resorption requires two phases: mechanical or chemical injury to the protective tissues and stimulation by infection or pressure.”
The Abstract classifies various types of root resorptions according to their stimulation factors:
• Pulpal infection resorption
• Periodontal infection resorption
• Orthodontic pressure resorption
• Impacted tooth or tumor pressure resorption
• Ankylotic resorption
We have found that a history of trauma including excessive occlusal loading and idiopathic pathology are also factors in external root resorption.
Treatment:
Fuss, Tsesis and Lin suggest that the selection of proper treatment is related to the stimulation factors and listed examples of treatment modalities, such as;
• Intrapulpal infection is the stimulation factor in internal root resorption and external periradicular inflammatory root resorption. Adequate root canal treatment controls intrapulpal bacteria and arrests the resorption process.
• Cervical root resorption infection originates from the periodontal sulcus and stimulates the pathological process. As adequate infection control in the sulcus is unlikely, removal of granulation tissue from the resorption lacuna and sealing are necessary for repair.
• Removal of the stimulation factor, i.e. pressure, is the treatment of choice in root resorption related to pressure during orthodontic treatment, or an impacted tooth or tumor.
• In ankylotic root resorption, there is no known stimulation factor; thus, no predictable treatment can be suggested.
We feel that once a diagnosis has been made, then treatment decisions may be determined. Because external root resorptions are complex and sometimes aggressive in nature, destruction of the root structure can vary from case to case and many times treatment recommendations are based upon whether or not the tooth is salvageable.
Common restorative products for resorption defects are hybrid glass ionomer composites, which have been found to be not only biocompatible with the subgingival environment, but the slow release of fluoride in the material reduces the risk of secondary decay.
Case #1: By John Y. Kwan, DDS
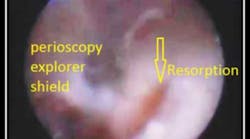
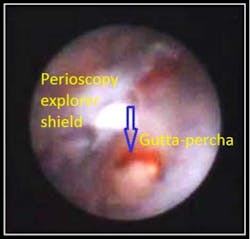
The below case and associated video is a Perioscopic view and debridement of an area of root resorption that clinically exhibited pocketing and bone loss.
This photo clearly demonstrates resorption which invaded so deeply into the root structure it exposed Gutta-percha which had been placed during a previous RCT.
Resorption which extends into the pulp chamber may require root canal therapy and in some instances, such as this case, the tooth may require extraction.
To view the video “Root Resorption,” see http://www.youtube.com/watch?v=aKqExI4EQ_s.