Endodontics vs. implants: understanding the possibilities of retreatment procedures -- part 2
Sept. 28, 2010
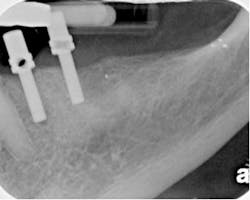
By Richard E. Mounce, DDSIn Part 1 of this two-part series, clinically relevant considerations regarding endodontic retreatment were made that provide the basis with which to discuss the following clinical endodontic retreatment cases. Four cases are detailed below to explain the technical challenges that will be encountered as well as treatment planning aspects of their clinical management. Case No. 1 The clinical case pictured in Figs. 1a to 1c was e-mailed to me for radiographic evaluation of the feasibility of retreatment. The patient was not examined clinically. An examination of the three radiographic angles of No. 29 is inconclusive with regard to the presence of radiographic pathology. The tooth has two roots and is posted and crowned. Radiographically, the crown lacks marginal integrity. If the crown and post were to be removed, this tooth would almost certainly show evidence of coronal leakage. The post appears centered in the lingual root. Because the patient was not examined, percussion, palpation, mobility, and probings were not known. The apical extent of the post is just below the crestal bone. The degree of bone support for the tooth is compromised with moderate to severe bone loss radiographically. Removal of the crown and post might provide evidence of vertical root fracture in the lingual root. It could be argued that because this tooth is asymptomatic, it could be left alone. While this might be a possible short-term strategy, it is not a viable long-term strategy. The prognosis for this tooth is hopeless as the remaining tooth structure after crown and post removal is not likely to be optimal. Another post would be required to rebuild the tooth. Even with an ideal retreatment, the long-term resistance to vertical fracture is compromised given the expected size of the new post, the remaining tooth structure, and the remaining bone support. The tooth was subsequently extracted. Case No. 2 No. 13 was evaluated for retreatment vs. extraction. The tooth had been treated approximately five years before and a separated file had been lodged into the apical third of the root. It appeared that an attempt had been made to remove the fragment at the initial treatment. The existing buildup appeared to terminate just below the cervical level of the tooth. The crown margins were open. The patient was symptomatic. The tooth was exquisitely percussion-sensitive, palpation-sensitive, slightly compressible in the socket, and probings were within normal limits. A mild to moderate buccal swelling was present. The tooth could be vertically fractured, but without probing to the apex, this could not be determined definitively without either dissembling the tooth or verifying after extraction. The prognosis for disassembling the previous root canal is very poor. Even if the crown were removed along with the buildup and the gutta percha evacuated, removal of the apical separated file fragment is not predictable. While it is technically possible that it could be removed, even if it were extracted without excessive dentin excavation, the resulting root would be highly at risk of long-term vertical fracture. When the above information was explained to the patient, the patient opted for extraction. Removal of the file fragment is highly complex because the portion of the file below the curvature could not be circumferentially touched with ultrasonic tips. In essence, it is impossible to get straight-line access to the body of the file given the canal curvature. It is conceivable that removal of the crown, amalgam, and gutta percha could have exposed the head of the separated RNT file and assisted its removal. But even so, this is not entirely predictable, even in the best clinical hands. If retreatment had been attempted and the root was not found vertically fractured upon access and the file was removed safely, this treatment would have required a two-visit treatment and an interim dressing of calcium hydroxide. Case No. 3The patient was symptomatic from No. 30 with localized discomfort. The tooth was sensitive to percussion and the buccal tissue sensitive to palpation. Mobility was slight and probings were within normal limits. The tooth had been treated when the patient was 11 years old, four years prior to appearing in my office. The initial treatment had failed to seal the mesial root apex. Given the dispersion of sealer in the mesial root, it was not entirely clear whether the root was vertically fractured or there were voids. The width of the preparation either represented excessive taper preparation or possibly sealer extrusion through a vertical fracture line. Treatment failure was caused by a lack of coronal seal and uncleaned and unfilled space that remained after the root canal. Retreatment was predictable in that once the uncleaned and unfilled space was addressed (correcting the defects present in the previous treatment) and a coronal filling placed, clinical success and periapical healing was highly probable. Disassembly of this tooth is predictable. Removal of the gutta percha was possible with heat, mechanical means, and solvents as a last resort as described in Part 1 of this series. The open apices at both the apex of the mesial and distal roots complicated removal of the existing gutta percha. Excessive use of force during the mechanical removal of gutta percha and/or chloroform could easily extrude materials and irrigation solutions beyond the apex of both roots. The gutta percha was removed and the shape of the canal preparations corrected to provide a continuous taper throughout the root length. The mesial root was filled entirely with RealSeal* bonded obturation master cones. The distal root had MTA (Dentsply Tulsa Dental, Tulsa, OK, USA) placed at the apex and RealSeal* extruded through the Elements Obturation Unit* above the apical third. A layer of flowable composite was placed over the pulpal floor to provide protection against coronal leakage before the buildup was placed. Case No. 4 No. 30 was asymptomatic with a mild and dull localized pain surrounding it. Preoperatively, the relatively straight white line at the apex of the mesial root was indicative of the fragment of a separated instrument. The previous treatment had taken place through the crown. Coronal seal was not established after the previous root canal. Treatment for this tooth required that the gutta percha be removed atraumatically with crown removal to facilitate straight-line access. Once the bulk of gutta percha was removed, efforts at achieving apical patency in the mesial root were undertaken using chloroform, one drop at a time, with small hand files to achieve patency by moving passively through the remaining gutta percha. Interestingly, in this clinical case, patency was achieved in both of the mesial canals, but the final obturation showed the same white line that was evident preoperatively. A second (previously untreated) canal was located, instrumented, and obturated in the distal canal. The tooth was sealed with a composite buildup. A two-part clinical series discussing possibilities for endodontic retreatment has been presented. Emphasis has been placed on visual and tactile control over the retreatment process, assessing restorability, treatment planning the post retreatment outcomes for risk of long-term vertical fracture, and strategic value of the tooth. In addition, the comparative success rate of implants vs. endodontic retreatment has been assessed.I welcome your feedback.*SybronEndo (Orange, CA, USA)
Richard E. Mounce, DDS, is the author of the nonfiction book “Dead Stuck” — “one man's stories of adventure, parenting, and marriage told without heaping platitudes of political correctness.” Pacific Sky Publishing. DeadStuck.com. Dr. Mounce lectures globally and is widely published. He is in private practice in endodontics in Vancouver, Wash. Contact him at [email protected].Figs. 1 through 4: Cases described in the text.
Fig. 1a
Fig. 1b
Fig. 1c
Fig. 2
Fig. 3a
Fig. 3b
Fig. 4a
Fig. 4b