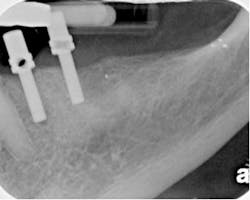
Fig. 1bFigs. 1a-1b: Upper first bicuspid that was accessed without a preoperative appreciation of the case difficulty. A near perforation resulted from the initial access. Subsequent treatment with the Twisted File* and RealSeal* bonded obturation.
Case 2: No. 5 was accessed and in the process, a near perforation occurred at the mesial. The clinician was unable to locate the canals and the case was referred mid-treatment. Evaluating the case reveals that the general practitioner who accessed this tooth did not appreciate the inherent challenges of this tooth. The risk of perforation initially is very high given the fact that access is being made through a bridge and the tooth is relatively narrow in a mesial to distal dimension. The bone loss at the cervical level also increases the long-term risk of vertical fracture. The clinician who accessed this tooth did not use the SOM. While a comprehensive discussion of this clinical case is beyond the scope of this article, suffice it to say that it was imperative that managing this kind of root and calcified canal system requires the clinician to remain in the long access of the root until canal location. The patient should be told of the risk of perforation and long-term vertical fracture before access is made. With the existing access landmarks obliterated, once the tooth was referred in this condition, it became imperative that canal location occur conserving as much dentin as possible. Once located, the canals required exacting management to prevent blockage and possible file separation among other iatrogenic events. Clinically this is accomplished using the following steps: 1) After the achievement of apical patency — when a hand K file reaches the minor constriction (MC) at the apex of each of the roots — the M4 Safety Handpiece* can be used to enlarge the canal to a diameter of a #15 hand K file. The M4 is a reciprocating handpiece attachment that reciprocates a hand K file 30 degrees clockwise and 30 degrees counterclockwise. This motion replicates the manual use of hand K files, saving hand fatigue, time, and in the process creating a more refined glide path than can be made by hand. As an aside, it may take significant time and a large number of hand K files to achieve apical patency. These hand K files should be precurved and can be trimmed to create a file that is stiffer than it would otherwise be, helping negotiate blockages and ledges. 2) After the glide path is created, it is essential that the clinician create the correct taper along the length of the root. Overzealous removal of dentin in taper preparation creates a long-term risk of vertical fracture. In this clinical case, the final prepared taper was a .08 taper to the apex prepared with the Twisted File* (with a .08/25 TF); the master apical diameter was prepared to a #40, again performed with the Twisted File. Once the canal was prepared to these dimensions, no evidence of vertical root fracture was found under the SOM. The tooth was obturated with RealSeal* bonded obturation material. See Fig. 2.
By Richard E. Mounce, DDSWhile it is hard to generalize, what I observe with rising frequency is a segment of the general dental population treating cases that are beyond their skill level and which should have been referred from the start. Giving at least 40 CE courses each year, I have a unique vantage point from which to observe this phenomenon on the American and global landscape. While it is unfair to make sweeping generalizations, my empirical opinion is well positioned at the ground level of the general dental market across the world. As I teach and travel, the evidence I see of this phenomenon is overwhelming. It is manifest as the doctors who tell me that they don’t refer at all, start every case, and then refer only when they are in trouble or only refer one or two teeth a year. Another manifestation of this issue is doctors who ask me how to treat complex trauma cases they are already involved in yet are unsure how to go forward. It appears from numerous contacts with such individuals that speed and profitability guide their actions.For obvious reasons, this is a problematic approach to endodontic treatment planning because it does not value either the patient or tooth retention. When viewed in this light, it is understandable why and how some oral surgeons and periodontists become cynical about endodontics and its success rate and become quick to recommend implants. As a practical matter, the legal and ethical standard of care should be the same between specialist and general practitioner. Across the widest spectrum of cases treated, there is not one standard of care. It is challenging to see how a general dentist (even with loupes) treating a challenging lower second molar with Gates Glidden drills, hand files, and a single-cone obturation technique can equal the result of an experienced endodontist with a surgical operating microscope (SOM) (Global Surgical, St. Louis, Mo., USA) and Twisted Files* and RealSeal* bonded obturation or some other combination of rotary system and warm obturation technique. With this as an identified problem, what are solutions?First off, one thing that is abundantly clear to me from teaching over the past seven years globally, there is very little comprehensive endodontic treatment planning training provided to either dental students or general dentists to help punctuate the lesson that referral is the best option when there is any doubt as to the clinician’s ability to achieve an excellent result. The particular treatment planning issues that could use illumination include an accurate set of criteria to both determine restorability and help identify iatrogenic risk factors preoperatively. In addition to these concerns, there is a whole subspecialty of cases that have already had root canal treatment whose clinical longevity needs evaluation. Knowing which cases can and should be re-treated is of significant clinical value. With the above ends in mind, a number of cases are discussed below. Case 1: The case was referred for endodontic treatment of No. 19 in order that the tooth might be hemisected and the distal root removed. Upon examination, No. 19 was sensitive to percussion, had mild buccal swelling, palpation sensitivity, and Class III mobility and pocketing to the apex of the distal root. Hemisection of No. 19 and removal of the distal root is virtually certain to lead to a vertical fracture of the mesial root of this tooth after root canal treatment and post build-up procedures. The patient was told that the tooth was not restorable and extraction planned. Had this tooth been treated with a root canal, its loss would have cost the patient significant funds and treatment time. These resources could have been put toward other options that would have provided the patient a better service. See Figs. 1a and 1b.